COVID-19 Update
Monday 06th June
Public Advisory
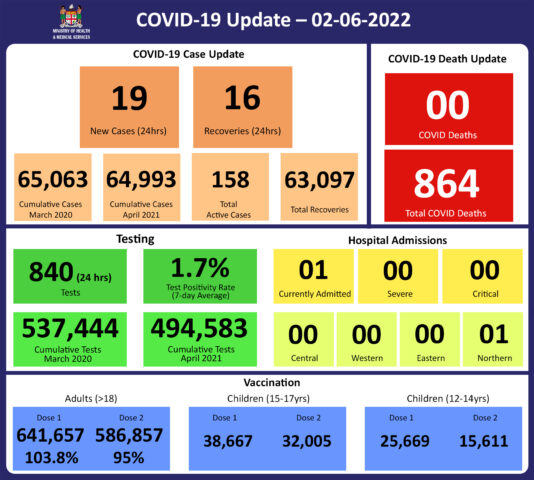
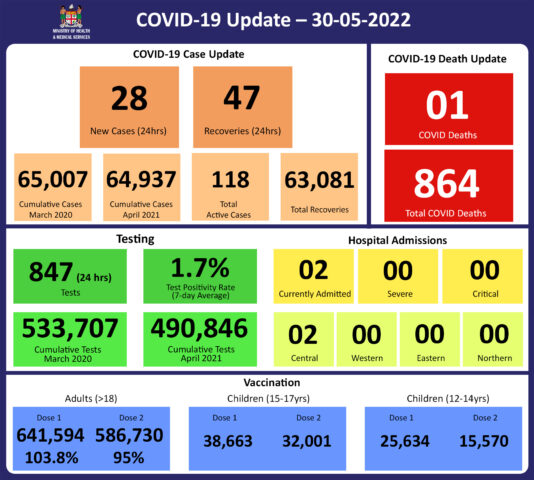
As of the 2nd of June, there was an increase in the number of people vaccinated by Moderna. We had also received backlog reports, hence we recorded a total of 134,042 individuals who received booster doses. We have also updated our booster eligible population. As such we report an updated booster coverage of 43%.
As of 06th June, a total of 134,719 individuals have so far received booster doses.
The months of April and May had recorded a low number of individuals getting boosters, this was represented in the initial booster coverage of 30.2% reported.
Increasing Vaccine Booster Coverage Program
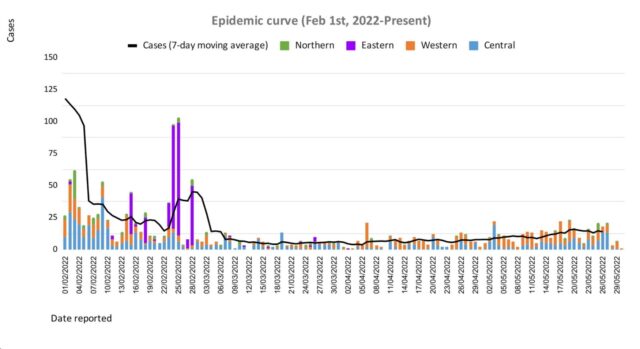
Currently, Fiji has COVID-19 primary series coverage of 95% and booster dose coverage of 30% for 18 years and over. It is well documented that immunity from COVID-19 vaccination wanes over time. The effectiveness of protection against COVID-19 after a primary series of AstraZeneca vaccination is lower than with other COVID-19 vaccine products, especially against the Omicron variant of concern. The current noticeable increase in cases indicates an urgency to increase our efforts to increase booster dose coverage. The return of most of the medical immunisation staff has also helped to ensure support for escalating our vaccine booster coverage program.
Based on this and international evidence the Ministry recommends the booster dose interval for eligible persons over 18 years be reduced to 3 months after the 2nd dose in recognition;
- of the risk of disease surge based on waning 2 doses of COVID-19 vaccine protection
- slow booster uptake
- increased international travel with the relaxation of border measures
- ongoing outbreaks in various parts of the world
Hence, we urge the public to get booster vaccine doses with a list of vaccination sites provided daily by the MHMS. Currently, both Pfizer and Moderna are recommended for booster doses.
In order to optimise coverage, the aim of the booster campaign is to administer 250,000 doses of Pfizer vaccine to those who have completed the primary series (doses 1 and 2) > 3 months prior but have not yet received a booster dose. This requires a minimum of 32,000 doses to be administered weekly for 8 weeks from 1 June to 31 July 2022. Based on the COVID-19 18 years + target population of 618,172 each division and subdivision will need to administer the number of doses outlined in Table 1 based on the 8-week target of 250,000 doses and weekly target of 32,000 doses.
COVID-19 booster priority populations are;
- Persons over the age of 18 years who have completed their primary series > 3months prior can receive their 1st booster dose
- Immunocompromised persons and those over the age of 60 years who had received the 3rd booster dose, may receive the 4th dose after a period of 4 months
- Health care workers, port staff, tourism and others who wish to receive a 2nd booster dose may receive it after an interval of 4 months from their first booster dose.
- Anyone over the age of 18 years who has taken their 1st booster dose can receive a 2nd booster dose after an interval of 4 months.
- Micro planning workshops commenced in the Central Division on 30th May 2022. Western and Northern Division will start on 6th June 2022. Follow-up supervisory visits will occur weekly until the end of June.
Risk Communication and Community Engagement (RCCE) will run parallel with the booster dose campaigns.
Planned Activities Include (but are not limited to):
- Discussion on information, education and communication materials including booklets, brochures, frequently asked questions pamphlets
- Promotional materials – pull up banners, stickers, sign boards for sites, network top-ups and Got my Booster water bottles and caps.
- Social media campaigns.
- COVID-19 booster drive/drive-through at markets, bus stands, events and faith-based organisations
- Radio messaging and announcements with daily targeted messages and sharing of vaccine site locations
- Community health worker training sharing information on booster doses
- Television advertisements
All these activities will be supported by MOHMS, South Pacific Community (SPC), United Nations Children’s Fund (UNICEF) and WHO.
International communicable disease outbreaks
As previously mentioned, the Ministry’s Fiji Centre for Disease Control (Fiji CDC) and Border Health Protection Unit (BHPU) are monitoring international outbreaks of concern, which include Ebola Virus Disease in the Democratic Republic of Congo, Japanese Encephalitis in Australia, acute hepatitis of unknown origin in multiple countries, and monkeypox in the United Kingdom and other countries. Where appropriate, specific interventions have been put in place or strengthened in response. The situation will continue to be monitored, assessed, and responded to based on the available scientific evidence, best practice, and advice from expert authorities.
Monkeypox
As we continue our recovery path during this pandemic, the strategies for resilience require urgent and early preparedness and response planning against any potential threat.
Monkeypox is a rare disease that is caused by infection with the monkeypox virus. It is endemic to certain countries in Central and Western Africa, and the causative virus is of the same family as the smallpox virus. Monkeypox outbreaks have been recently reported in a growing number of countries that are not endemic to the disease, including the United Kingdom, Spain, Portugal, France, Italy, Germany, Sweden, the Netherlands Canada, the United States of America, and Australia.
Monkeypox is usually a self-limiting illness, which means that most people recover with just supportive treatment within several weeks. However, severe illness can occur in some individuals. It does not spread easily between people but person to person transmission may occur through:
- contact with clothing or linens (such as bedding or towels) used by an infected person
- direct contact with monkeypox skin lesions or scabs
- exposure to respiratory droplets eg coughing or sneezing
The Ministry working with communications and community engagement teams has produced public advisories to help arm ourselves with the knowledge to protect ourselves and to help reduce the chances of spread in our community. Infection prevention protocols have been put together at the border and in community facilities. Protocols have been initiated to maintain oversight over travellers from selected countries to ensure early diagnosis, treatment, and contact tracing. The public advisories have covered symptoms to facilitate self-early diagnosis and information on transmission.
All doctors and Nurses in the community need to ensure they are well informed of how cases present and be vigilant in helping to ensure cases are diagnosed early.
The major priority for the Ministry of Health and Medical Services is to have a response plan that will include surveillance with rapid response and containment protocols and at the same time have a minimal social and economic impact. A key focus will be on ensuring that those suspected or confirmed to have monkeypox must be able to be managed in a dignified manner with no threat of stigmatisation. Each citizen’s duty to contribute to protecting Fiji must be the priority.
We are in discussions with our reference laboratory in Melbourne to ensure access to definitive tests. Our ongoing efforts to have genomic sequencing capability in the Fiji CDC will provide us with greater capacity to deal with infection threats now and in the future.
We are also in discussions with WHO to ensure we preposition access to vaccines and medications used to treat monkeypox.
However, it is important to ensure that in escalating community-wide infection prevention and control measures, we are responding to current threats and creating community-wide resilience to upcoming threats. Our ongoing engagement in a healthy lifestyle to mitigate NCDs is also part of the overall focus on building back better and stronger.
The Ministry of Health and Medical Services will CONTINUE TO disseminate more specific advisories over the next few days to weeks. Further updated knowledge about the monkeypox virus will be shared as they are known.
Ongoing Medical Recovery Efforts
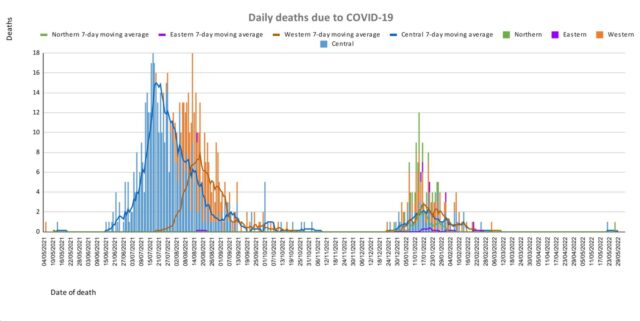
With reducing COVID-19 cases and people presenting to health centres with acute respiratory illness, the MOHMS team is better positioned to focus more on health facilities and health care provision capabilities to mitigate against severe disease and death. This will include the ongoing community engagement and outreach program to facilitate early diagnosis and treatment in the community, and the maintenance of health facility readiness to provide treatment.
Our command and operation centres have been repurposed to maintain a line list of vulnerable cases in the community and work on processes that will allow for more preemptive response and promote broader community resilience. These command centres and operation centres will also provide oversight on community surveillance indicators to ensure early and measured responses to future outbreaks.
We are also focused on carrying out general health service work more efficiently in all facilities, and a key part of our plan is to set up divisional mobile units to supplement facility-based general servicing capability and also work with private providers through a process for pre-qualifying contractors and/or suppliers for each subdivision.
The engagement of General Practitioners, Private Dental Practitioners, Private Medical Laboratories, and Private Ambulance providers to support our services in a public-private partnership arrangement is a strategy to help in our ongoing recovery efforts.
We also have reformulated a framework to better engage customer service initiatives in all health facilities and allow for senior managers to institute substantive actions and provide direct oversight over implementation plans. It will also allow the Ministry’s senior executives to track progress in implementation and ensure that annual operation plans reflect an evolving and progressive change narrative in the successive plans. These initiatives will also include the processing of internal communications to facilitate timely decision making and action within the Ministry.
COVID-19 Vaccination
The booster dose interval for eligible persons has been reduced to 3 months from the 2nd dose. This is in recognition of the risk of disease surge based on waning 2 doses covid vaccine protection, slow booster uptake, increased international travel with the relaxation of border measures, and ongoing outbreaks in various parts of the world. Moderna vaccine and Pfizer vaccines are both available for adult booster doses.
We have commenced administering the second COVID-19 booster dose to the eligible population who are aged 18 years and above. They can get the second booster after an interval of 4 months from receiving their first booster dose.
The public is urged to get booster vaccine doses, and the list of vaccination sites is provided daily on the MOH. We have accepted an offer of 50,000 doses of Pfizer paediatric doses for children aged 5 to 11 by the Aotearoa New Zealand Government.
Our school vaccination program has also been progressing such that with the 95% adult coverage rate, 90.6% of all persons over 12 years have had 2 doses of the COVID-19 vaccine.
We will continue to monitor the evidence on post-infection immunity based on quality data generated globally. However, until we have a better sense of the role of post-infection immunity, the Ministry of Health will continue to define our level of protection based on vaccination numbers.
Given the current stocks of Pfizer vaccines, we are now covering the Primary doses for those yet to be vaccinated and for Dose 2 if individuals were vaccinated with either Moderna or AstraZeneca while the 12-14-year-olds continue with the Pfizer vaccine.
Cold and flu
The Ministry of Health and Medical Services has noted an increase in people becoming ill with cold and flu-like illnesses as we are coming into our dry and cold season. This increase is especially seen in infants and children under the age of 5. The paediatrics department at CWM Hospital is also seeing an increase in children under the age of 5, especially infants, being admitted with acute respiratory illnesses while testing negative for COVID-19 and influenza. It has been expected that as restrictions intended to prevent transmission of COVID-19 were lifted (including mandatory masking, physical distancing, and school and border closures) other respiratory viruses that normally circulate would begin to re-emerge similar to pre-COVID levels, and possibly even at higher levels due to a decrease in population immunity to seasonal viruses, as cold/flu cases were low during the last two years.