COVID-19 Situation Update
Wednesday 09th February
| Transmission Update:
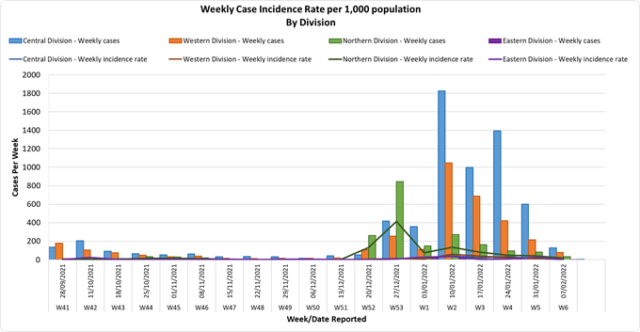
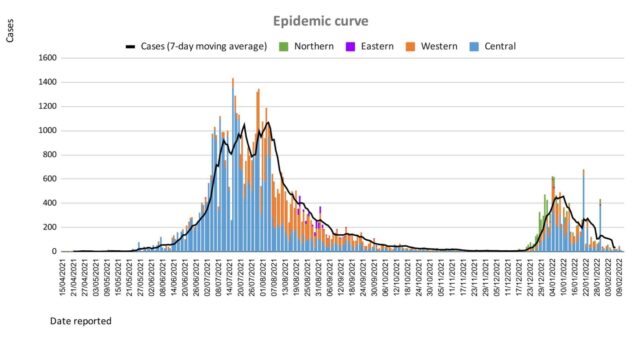
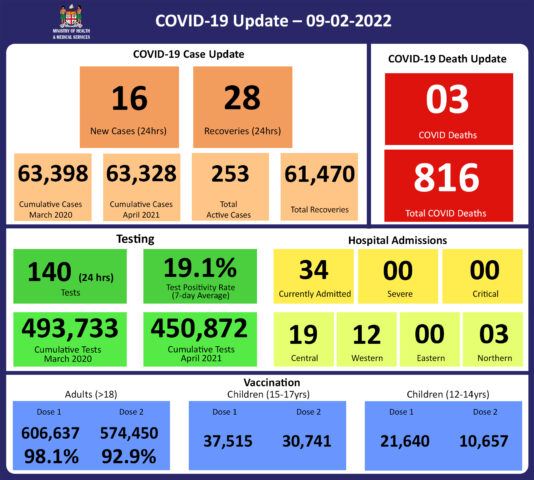
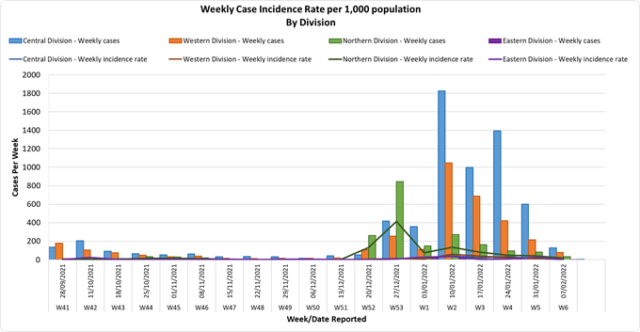
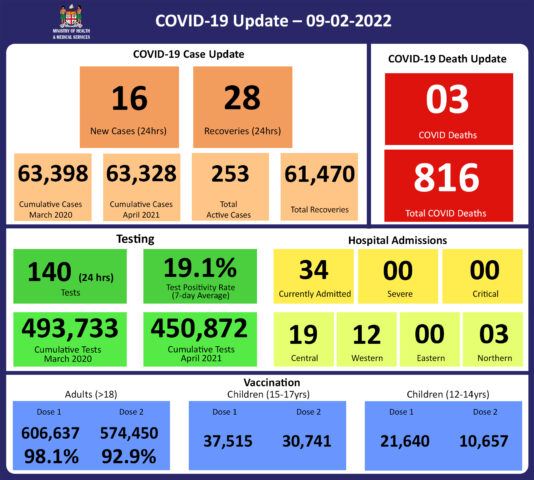
Since the last update, we have recorded 36 new cases of which 20 new cases were recorded on 08/02/2022, and 16 new cases in the last 24 hours ending at 8 am this morning.
Of the 36 cases recorded, 25 cases were recorded in the Central Division; 11 cases were recorded in the Western Division, nil cases were recorded in the Northern Division, and nil cases were recorded in the Eastern Division.
The national 7-day rolling average of cases as of 5th February is 95 daily cases.
In the 7 days until 08/02/2022, 107 new cases were recorded in the Central division, 67 new cases in the Western division, nil new cases in the Eastern Division, and 27 new cases in the Northern Division.
The Central Division cases constitute 68% of the cumulative total cases nationally, with the Western division making up 28%, 3% in the Northern Division, and 1% in the Eastern Division. |
| Deaths:
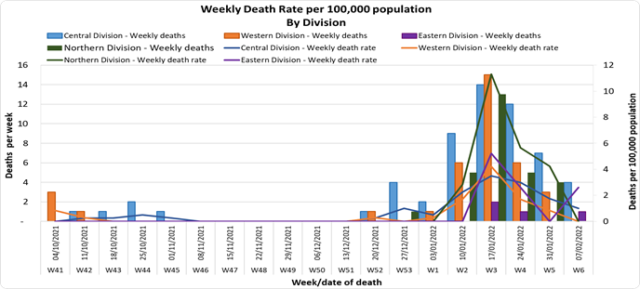
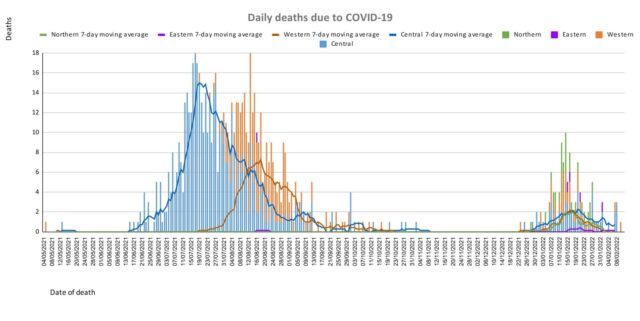
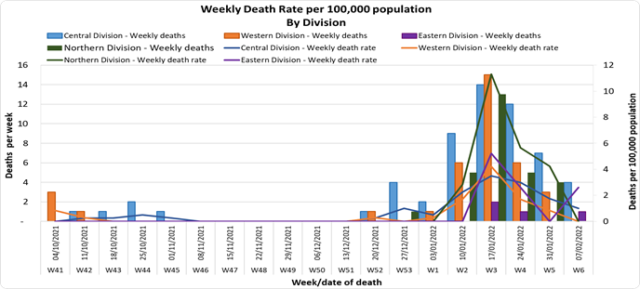
This graph depicts daily COVID-19 deaths by division since May 2021. It indicates a surge from mid-December 2021, which peaks by mid-January 2022. It is from this time period when the 3rd wave had started (Note: Death notifications from the week of 24/01/22 and 31/01/2022 are still being received, we are currently on week 07/02/2022, therefore the appearance of a downward trend on the graph from week 31/01/22 may not be accurate. There are deaths from the Western Division currently under investigation for the same time period hence, the death rate for the division may increase).
Analysis of Deaths in the Third Wave
Table 1: Death rates by Division
| Division |
Total COVID Deaths |
Deaths per 100,000 |
| Central |
56 |
13.9 |
| Western |
32 |
9 |
| Northern |
28 |
20.0 |
| Eastern |
4 |
10.4 |
An analysis of the 120 deaths recorded in the third wave show that, while the Central Division has the highest absolute number of deaths, the Northern Division has the highest rate of death when adjusted by per 100,000 population. (Note: There are deaths currently being investigated from the Western Division for the same time period, therefore the rate for the division may increase).
Table 2: Deaths by Age Group
| Age Group |
Total Deaths |
Deaths per 100,000
population |
| 0 – 9 |
5 |
2.7 |
| 10-19 |
2 |
1.3 |
| 20-29 |
3 |
2.1 |
| 30-39 |
3 |
2.2 |
| 40-49 |
5 |
4.8 |
| 50-59 |
17 |
18.7 |
| 60-69 |
25 |
48.1 |
| 70-79 |
36 |
160.7 |
| 80-89 |
20 |
355.4 |
| 90-99 |
4 |
769.2 |
For the 120 deaths in the third wave, the death rate adjusted per 100,000 population, has been highest in age groups 50 and onwards. There were 7 deaths below the age of 19 years, 6 out of the 7 children had significant pre-existing medical conditions, and one child had no known underlying medical condition.
Table 3: Deaths by Vaccination Status
| Age Cohort |
Total COVID deaths |
Total Vaccinated/
Unvaccinated |
Deaths per 100,000 Vaccinated Population |
Deaths per 100,000 Unvaccinated Population |
| >18 |
113 |
50/63 |
8.7 |
144 |
| 15-17 |
1 |
0/1 |
0 |
6.6 |
| 12-14 |
1 |
0/1 |
0 |
2.5 |
Out of 120 COVID -19 deaths reported in the third wave, five (5) deaths were in the population not eligible for vaccination (under age 12). An analysis of the 115 deaths in the vaccine-eligible population reflected that when adjusted per 100,000 population, for fully vaccinated (received 2 doses) and unvaccinated/not fully vaccinated (received 0 doses or only 1 dose) adults in Fiji, a death rate of 8.7 per 100,000 population for fully vaccinated adults and 144 for unvaccinated adults was exhibited. This means that unvaccinated adults in Fiji have been dying at a rate 16.5 times higher than fully vaccinated adults during the current COVID-19 wave. Individuals of the 12-17 age group who died were not vaccinated. There have been no COVID-19 deaths in individuals who received a booster (3rd dose) of the vaccine.
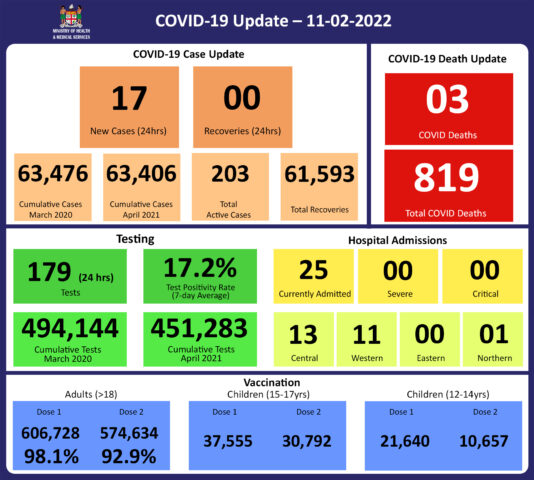
New deaths to report
There are 3 new COVID-19 deaths to report from the 7th and 8th of February, 2022.
The first COVID-19 death to report is of a 59-year-old male from the Central Division, who was admitted at the CWM hospital on 12/01/2022. His pre-existing medical conditions contributed to the severity of his illness and he sadly died on 07/02/2022. He was fully vaccinated.
The second COVID-19 death to report is of a 64-year-old male from the Central Division, who was admitted at the CWM hospital on 14/01/2022. He sadly died on 07/02/2022 and was fully vaccinated.
The third COVID-19 death to report is of a 55-year-old female from the Central Division, who was admitted at CWM hospital on 28/01/2022. She sadly died on 08/02/2022 and was fully vaccinated.
There has been a total of 816 deaths due to COVID-19 in Fiji. Please note that due to the time required by clinical teams to investigate, classify and report deaths, a 4-day interval is given to calculate the 7 days rolling average of deaths, based on the date of death, to help ensure the data collected is complete before the average is reported. Therefore, as of February 5th, 2022, the national 7 days rolling average for COVID-19 deaths per day is 0.9, with a case fatality rate of 1.29%.
We have recorded 857 COVID-19 positive patients who died from other serious medical conditions unrelated to COVID-19; their doctors determined that COVID-19 did not contribute to their deaths, therefore these are not classified as COVID-19 deaths. |
| Hospitalization:
There is a downward trend in daily hospitalizations. Using the WHO clinical severity classification, a greater percentage, 68% (n=23) of the admissions of COVID-19 positive patients are categorized as asymptomatic and mild, 14% (n=5) are categorized as moderate and 18% (n=6) as severe with nil case in the critical category. Anyone admitted to the hospital is tested before admission, therefore, a significant number of people are admitted to the hospital for non-covid health conditions, but incidentally, test positive due to the high amount of transmission in the community. The number of people being admitted because of COVID-19 remains low. |
| Testing:
140 tests have been reported for February 8th, 2022. Total cumulative tests since 2020 are 493,733 tests. The 7-day daily test average is 172 tests per day or 0.2 tests per 1,000 population.
The national 7-day average daily test positivity is 19.1%. The high positivity rate is an indication of widespread community transmission. |
Public Advisory:
On Sunday 6th February we saw the announcement of the lifting of a number of public health and social restrictions. As we transition into reducing the legal premises for the enforcement of COVID Safe measures, it is expected that there will be a community-wide engagement of the COVID Safe measures in a sensible manner. The measures we have continued to emphasize are ventilation, masking, physical distancing, cough/sneeze etiquette, hand washing, and isolating from others if you have symptoms.
Hand washing and cough etiquette are immovable as public health measures. Regular hand sanitization and coughing/sneezing into a tissue or handkerchief, or the bend of your elbow, are healthy habits that protect yourself and others from COVID-19 and other infectious diseases. Isolating yourself, or staying away from others, when you are sick with any respiratory illness is also a good habit to protect others, especially the vulnerable.
Masking, physical distancing, and ventilation are 3 measures that must constantly be present, but there is some flexibility in increasing 2 others when one of the measures becomes difficult to apply. Whatever the scenario, an effective mask must be kept close to you at all times. The current masking requirement that wearing a mask that covers your nose and mouth is mandatory in all public places for everyone aged 8 and over, including in public service vehicles remains in force. The Ministry of Health and Medical Services is looking into a list of exemption criteria; however, we expect that this list will not be exhaustive and we hope to leave some space for a common-sense approach to evolve.
In a setting where physical distancing of 2 metres is more difficult, then increasing ventilation and more strict masking practice will be needed even more. A well-ventilated indoor space refers to an indoor space wherein there is a good movement of outside air coming into the space, and inside air is going out. A suboptimally ventilated space is bad for many reasons aside from COVID, however, in this scenario, the physical distancing rules will increase and masking is more necessary. For custodians of workplaces, houses of worship, and the like, balancing the relationship between ventilation, physical distance, and masking is the only way to ensure that services are COVID safe and can be customized to the principle of living with the virus. SOPs need to be configured to all activities that occur in your work or worship space in order to be COVID Safe resilient. We all want to mitigate the risk of unsustainable sick leave levels every time we get a variant, and more variants will come. Mitigating the risk of people getting sick is the best way to reduce further the risk of severe disease and death beyond the protection afforded by vaccination. Promoting good COVID safe principles in a common-sense approach is the best way to start; for example, it is clearly obvious that social dancing in an open outdoor space is much safer than social dancing in the confines of a nightclub.
Again, we wish to emphasize that the legal mandates and restrictions that were put in place to promote COVID safe measures in addition to the usual health promotion activities (posters, mainstream, and social media messaging, etc), are traditionally used to help rapidly turn COVID Safe measures into COVID Safe Habits. While the mandates were urgent and necessary, the ultimate objective is to build a platform for a good sense approach on how we turn healthy measures into healthy habits.
The tragedy of the deaths from COVID-19 is a sad reminder of the impact of this pandemic, however, the bigger tragedy is if all the very obvious lessons we have repeatedly published, announced, and posted on social media are too quickly forgotten. The Vaccine Plus approach must become a personal daily objective and the COVID safe measures become a community-wide habit, for us to safely navigate to a more secure socioeconomic future.
While we have reported that fully vaccinated people have died during this third wave, deaths in unvaccinated people (in the vaccine eligible population) are occurring at over 17 times the rate of the vaccinated. This confirms what we already know from other countries, which is that vaccination reduces the risk of severe disease, hospitalization, and death from COVID-19. The fact that we still have people not fully vaccinated, especially people who are at high risk of severe disease and death (the elderly and people with chronic diseases including NCDs) remains a serious concern. And we would strongly urge everyone, especially medical professionals, to encourage and promote vaccination.
Vaccination
We have noted how difficult it is to increase our vaccination coverage for the last 10% of our adult population despite the increased risk of severe outcomes in this group. While we will continue to do our part to promote and deploy vaccines, we need community support to sustain the impact of our efforts especially to the vulnerable within this 10%. It is a grave concern that we continue to receive requests for vaccine exemption from persons with medical comorbidities, especially NCDs; their medical condition is an indication for vaccination, and granting the exemption is not an option for any qualified medical person.
The booster dose program began at the end of November 2021. As of January 31st, 83908 individuals have so far received booster doses of the Moderna COVID-19 vaccine. For the month of February, a further 175,558 have become eligible for booster doses. We are targeting to cover all these eligible individuals in the days ahead.
Health Services Transition
The implications of COVID-19 to health service provision are clear. The required change in the health service delivery model implies a change to infrastructure, human resource structure, working conditions, equipment, and the supply chain of drugs and consumables.
One important change that will require community-wide support is in developing the capability to ensure that available health care services get to those who need the service. We will continue to collaborate with our development partners, other government ministries, faith-based groups, and civil society organizations to enable our reach into communities.
With the pandemic into its second year, the Ministry has maintained emergency mode operations for much of this time. There is an urgent need to safeguard the welfare of our medical staff by ensuring that they get some rest and attend to family needs. As such we will embark on initiatives to ensure that our staff moves back to working normal working hours, take official leave entitlements accrued over the past year, and receive payment of meal and other allowances they are entitled to. We will continue to look at sustainable options to support our medical staff in working within the scope of our remodeling of health service delivery. However, we do anticipate that this will need to be part of a medium to long-term plan for the Ministry.
We have also highlighted how severe comorbidities and poor health-seeking behaviour have vastly contributed to severe outcomes in the COVID outbreak. We need to build resilience in the face of an endemic problem. Based on the lessons learned from the deaths, we need to:
- Prevent all preventable chronic diseases of which NCDs are the most prominent
- Promote the better control of controllable chronic diseases of which NCDs are the most prominent, and
- Build stronger support for better health-seeking behaviour especially among the vulnerable amongst us
We are urgently reviewing and strengthening our public health measures to find, stop and prevent health threats wherever they arise. Our sub divisional health teams have been reminded to review and strengthen their community surveillance program and line list management of vulnerable persons.
However, the impact of these efforts cannot be sustained unless we get a broad level of support from the community in implementing the above 3 strategies, and at the same time reducing the transmission of COVID-19 to protect our vulnerable populations. Maintaining the Vaccine Plus approach remains critical.