Last Updated on 1 year by Publishing Team
COVID-19 Update
Thursday 08th December
| Transmission Update:
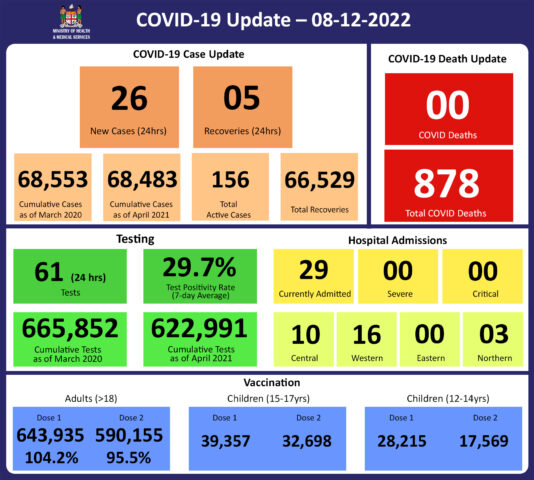
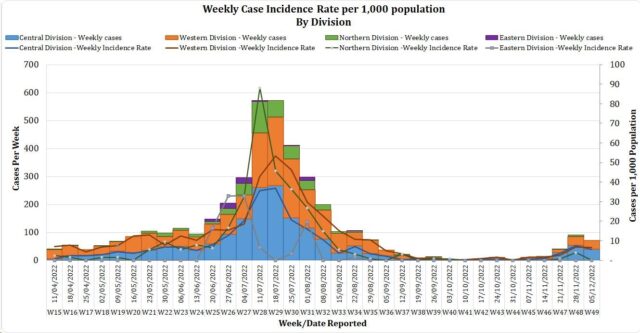
Since the last update on 01/11/2022, we have recorded 102 new cases and 10 reinfections. Of the 102 new cases recorded, 70 cases were recorded in the Central Division; 32 cases in the Western Division; with nil cases in the Northern and Eastern Divisions. Of the 10 reinfections recorded, 6 cases were recorded in the Central Division and 4 cases in the Western Division. The national 7-day rolling average of cases as of 4th December is 10 daily cases. The Central Division cases constitute 66% of the cumulative total cases nationally, with the Western division making up 28%, 4% in the Northern Division, and 2% in the Eastern Division. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Deaths:
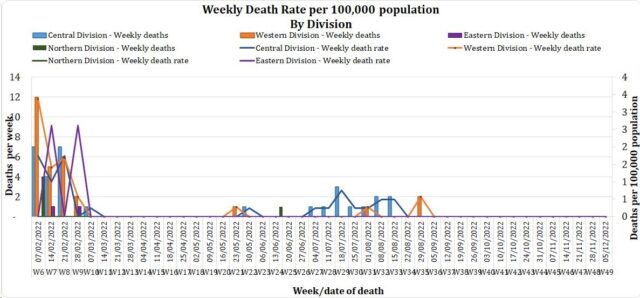
The curve depicts weekly COVID-19 deaths by division since May 2021. It indicates a surge from last December, with peaks in mid-January 2022 followed by a downward trend. COVID Death Reports We have no (0) new COVID-19 deaths to report. Analysis of COVID-19 Deaths Table 1: Death rates by Division
The curve depicts weekly COVID-19 deaths by division since May 2021. It indicates a surge from last December, with peaks in mid-January 2022 followed by a downward trend. Table 2: Deaths by Age Group
For the 177 deaths since December 2021, the death rate adjusted per 100,000 population, has been highest in the age group 50 years and over. There were 10 deaths below the age of 19 years, 7 out of the 9 children had significant pre-existing medical conditions, and three (3) children had no known underlying medical condition. Table 3: Deaths by Vaccination Status
Of the 177 COVID-19 deaths reported since December 2021, eight (8) deaths were in the population not eligible for vaccination (under the age of 12). An analysis of the 169 deaths in the vaccine-eligible population revealed that Fiji has a death rate of 11.7 per 100,000 population for fully vaccinated adults and 333.6 per 100,000 population for unvaccinated adults. This means that unvaccinated adults in Fiji have been dying at a rate 28.5 times higher than fully vaccinated adults. Individuals in the 12-17 age group who died were not vaccinated. There has been a total of 878 deaths due to COVID-19 in Fiji. As of August 18th, 2022, the national 7 days rolling average for COVID-19 deaths per day is now 0.0, with a case fatality rate of 1.29%. Due to the time required by clinical teams to investigate, classify and report deaths, a 4-day interval is given to calculate the 7 days rolling average of deaths, based on the date of death, to help ensure the data collected is complete before the average is reported. We have also recorded 998 COVID-19-positive patients who died from other serious medical conditions unrelated to COVID-19; their doctors have determined that COVID-19 did not contribute to their deaths, and therefore these are not classified as COVID-19 deaths. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Hospitalisation:
Currently, we do not have any (0) admissions as a direct cause of COVID-19. However, twenty-nine (29) admissions have tested as covid positive but are admitted for other diseases. Patients presented to the hospital are tested before admission therefore, a high number of people who are admitted for non-covid health conditions, test positive for COVID-19 due to the current level of transmission in the community. Using the WHO clinical severity classification, there are 83% (n=24) cases in the asymptomatic and mild categories; 10% (n=3) cases in the moderate; 7% (n=2) in the severe category with nil cases in the critical category. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Testing:
61 tests have been reported for December 7th, 2022. The total cumulative tests since 2020 are 665,852 tests. And the 7-day daily test average is 48 tests per day or 0.1 tests per 1,000 population. The national 7-day average daily test positivity is 29.7%, which is above the WHO recommendation of 5% and indicates the ongoing community transmission in Fiji. |
Public Advisory
For COVID-19;
We are once again noting an increase in COVID-19 cases based on case numbers reported to us, positivity rates being compiled from hotel, airport and hospital workers and absenteeism rates from selected industries and schools. We have registered 29 patients who have incidentally tested positive for COVID-19 while being admitted to the hospital. Correspondingly, we are currently focusing on implementing COVID safe measures around those vulnerable to the severe effects of COVID-19. This includes escalating measures in hospitals, old people’s homes and facilities catering for disabled persons. As such we expect to escalate screening protocols and masking for staff, patients and visitors. Furthermore, visitor restrictions will be in place.
Consistent with the experience in other countries that have high vaccination rates, we anticipate a minimal increase in hospital admissions for COVID-19 disease despite increasing case numbers. While immune protection from the severe disease remains, there is expected to be some immune escape capability that makes the variant more transmissible.
For the general public, we are advising that COVID safe measures need to be instituted around the elderly, those with chronic disease, pregnant mothers and children with disabilities. This involves proper masking of those caring for vulnerable persons, safe physical distancing for those visiting them, and ensuring they engage in highly ventilated spaces when they venture out of their homes. It is important for those with chronic diseases to be on proper treatment that ensures the optimal control of the diseases they have. This means that diabetics need their blood sugar to be as near normal as possible, hypertensives need their blood pressure well controlled and those with cardiac conditions to be as symptom-free as possible.
We emphasise the point that strengthening our ability to live with COVID means we remain vigilant, maintain community-wide adoption of COVID safe measures where appropriate, and maintain the impetus for immunisation This is the only means to reduce the disease spread and protect those in the community who are less able to fend for themselves.
Prior to noting this increase we had initiated the rescinding of some COVID-related public health measures relating to nightclubs, churches, sporting events and high-risk businesses. The decision to relax public health measures is based on the low number of admissions and severe cases despite the current changes in case numbers. We believe that the planned relaxation of public health measures will not have any adverse effect in terms of the number of severe COVID cases we expect to see from the recent increase in case numbers.
LTDD
We have noted rising trends in cases of Leptospirosis and Dengue however our admission levels remain low and the mortality rate among admitted cases remains low. This is despite the fact that our reported case numbers had remained near or slightly above the outbreak level for most of this year. We acknowledge the efforts of our community leaders, community health workers and health workers in the primary health space for their efforts in facilitating early detection and treatment. Also, our divisional health teams with the support of staff from the National Disaster Management Team have been carrying out pre-emptive source reduction measures in selected hotspots over the last month.
Recent heavy rain and flooding have affected many areas and communities throughout the country. The Ministry is focussing on geographical areas of concern for the purpose of mobilising extra capability to help manage communicable disease outbreaks and also escalate the promotion of preventative measures.
To reduce your individual risk, it is important to understand that exposure to animals, soil, mud, and floodwaters during work or recreation activities increases your risk of infection.
Important prevention measures include wearing fully covered footwear at all times when going outdoors, avoiding wading or swimming in flooded waters, using clean fresh water to wash up after exposure to muddy waters, and keeping all food and drinks covered and away from rats. For workplaces, practise good personal hygiene at all times, cover cuts and wounds well, and use protective equipment, especially footwear when in flooded and muddy areas.
Early treatment can decrease the severity and duration of the disease. Please seek medical care if you have recently had contact with floodwaters, mud, or animals, and develop the following symptoms: fever, muscle pain, and headache. You may also have red eyes, loss of appetite, nausea/vomiting, dizziness, or feel weak.
Leptospirosis can be treated with appropriate antibiotic medications prescribed by a doctor if treatment is sought early. Danger signs for severe leptospirosis include shortness of breath, coughing blood, chest pain, yellow eyes/skin (jaundice), signs of bleeding (including unexplained bruising), decreased or increased urination, and difficulty staying awake. Severe leptospirosis is life-threatening, and anyone with these symptoms must be taken to the hospital immediately.
The Ministry has reported an outbreak of Typhoid in the Raranibulubulu community in Vanua Levu and sporadic cases in Navosa. Measures taken so far through outreach deployment of medical teams and the effective efforts of community leaders have controlled any escalation in case numbers. Typhoid fever is typically found in areas that do not have access to clean drinking water. We strongly encourage people who live in rural areas, informal urban areas, and any other areas where access to clean drinking water is limited, to boil all drinking water. We must all also continue to practise basic hygiene measures such as frequently washing hands with soap and water, especially after visiting the toilet and before eating or preparing food.
Mitigating the Ongoing Exodus of Medical Staff
The ongoing exodus of medical staff has been highlighted and remains a challenge in terms of our ongoing effort to rebuild better and stronger. It is part of a global phenomenon, and as such short-term and long-term mitigation measures are needed.
Our immediate measure involves supporting the development of a support cadre of workers by relooking at new programs that support lower-tier health cadres with shorter-duration training programs which at the same time provide alternative entry points to medical professions. We already have a community health worker program. We are reviewing a program for nurse aides, and also exploring a theatre technician training program to support our efforts to support broader access to safe surgery and looking to recruit graduates from medical programs who can provide support roles to nurses and doctors. We have also redesigned an easier and faster process of engaging volunteers through our volunteer support program to cater for those in urgent need for work experience.
The Ministry continues to review and employ strategies to improve the working environment of our workforce.
- A 12-hour roster system is being strategically implemented in some settings.
- We are finalising discussions to at least partially pay for pending leave to maintain health staff numbers.
- We are also increasing the clerical officer cadre in large health centres and hospitals to reduce the administrative workload on the medical staff.
- There are staff shortages that entail some health workers staying long hours at work however, we have redeployed more finance into the overtime and meal allowance allocation and using the time off in lieu condition to help to mitigate this.
- We have evolved a network of command centres that will optimise network communication to maintain surveillance on key issues and ensure that action plans are implemented well to mitigate those issues. Quality care improvement is an important cornerstone in all action plans.
- We have good in-country stocks of medicines and consumables and we have strengthened our distribution capability to ensure better stock availability in health facilities. We expect that once we have put in place warehouse capability in the Northern and Western Divisions we will see a marked improvement in this space.
A government-wide customer service initiative is also a key part of the command centre work plans. These initiatives will also include processing internal communications to facilitate timely decision-making and action within the Ministry. It will also allow the Ministry’s senior executives to track progress in implementation and ensure that the annual operation plans reflect an evolving and progressive process.
Furthermore, we continue to support the government’s initiatives for greater engagement between the public health sector and the private health sector to mitigate potential service gaps caused by the ongoing migration. This includes the engagement of General Practitioners, Private Dental Practitioners, Private Medical Laboratories, and Private Ambulance providers to support our services in a public-private partnership arrangement.
In the medium, to long term, the remuneration packages for medical staff will need to be adjusted to foster retention. This has started with Laboratory technicians being transitioned to laboratory scientists at a higher salary level, enrolled nurses being transitioned to nursing assistants at a higher salary level and raising the entry salary level for pharmacists. Budget submissions have been prepared and are being prepared to support human resource expansion and remuneration.
COVID-19 Vaccination
We have been reporting that 100% of our estimated adult population have received one dose and 95% have received the second dose. The vaccination of our target population has been progressing well with the 12 years and above coverage rate for Fiji being 99% for Dose 1 and 89% for Dose 2. Furthermore, as of the 08th of December, 170,060 (54.4%) booster-eligible individuals have so far received their 3rd dose while 28,720 individuals have been administered the 4th dose.
Increasing Vaccine Booster Coverage Program
We urge the public to get booster vaccine doses at the vaccination site closest to them and the list of sites is provided daily by the MHMS. Currently, both Pfizer and Moderna are recommended for booster doses.
To optimise coverage, our current target of the booster campaign is to administer 250,000 doses of the Pfizer vaccine to those who have completed the primary series (doses 1 and 2) three or more months prior but have not yet received a booster dose.
COVID-19 booster priority populations are;
- Persons over the age of 18 years who have completed their primary series > 3 months prior can receive their 1st booster dose
- Immunocompromised persons and those over the age of 60 years who had received the 3rd booster dose, may receive the 4th dose after a period of 4 months
- Healthcare workers, port staff, tourism and others who wish to receive a 2nd booster dose may receive it after an interval of 4 months from their first booster dose.
- Anyone over 18 years who have taken their 1st booster dose can receive a 2nd booster dose after an interval of 4 months.