Epidemic Outlook:
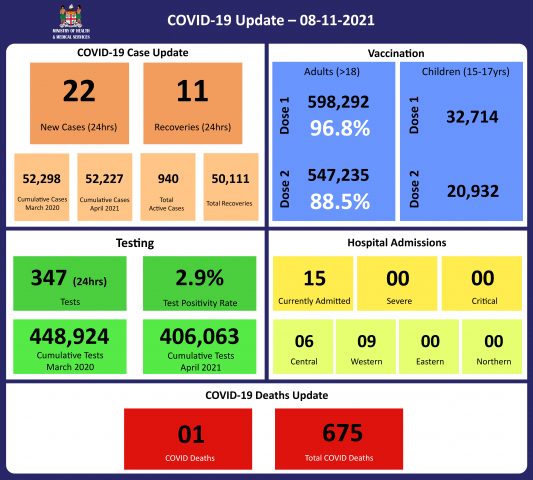
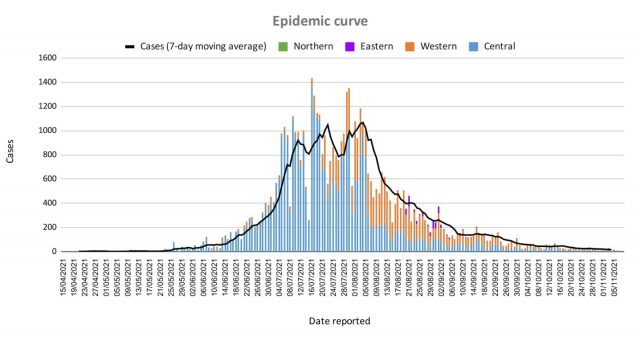
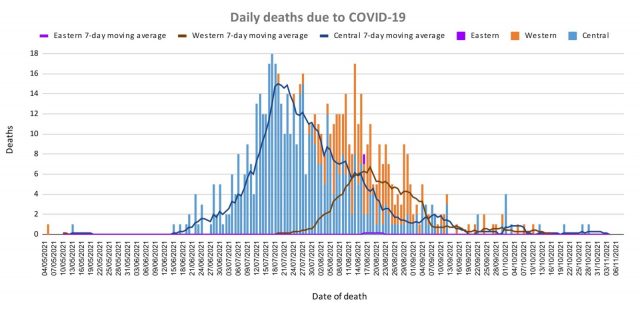
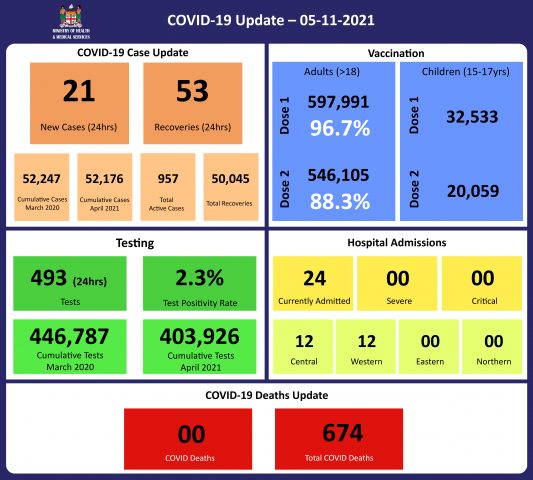
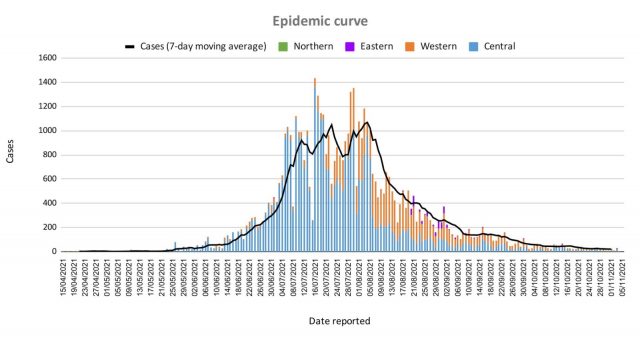
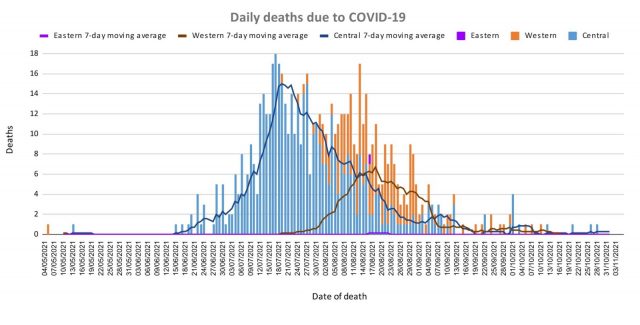
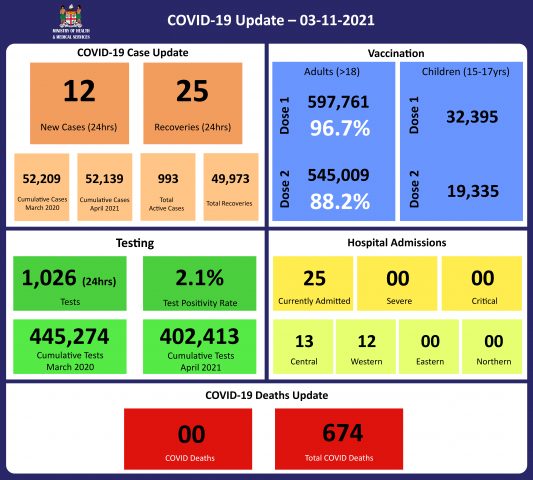
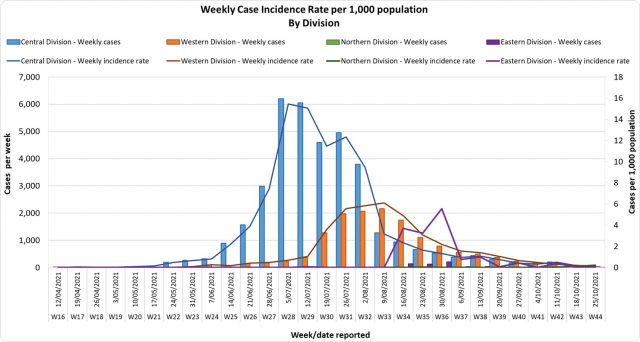
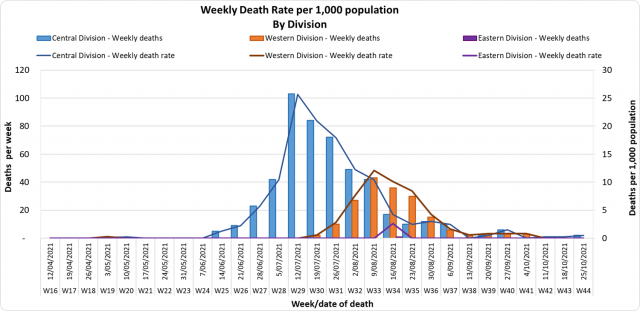
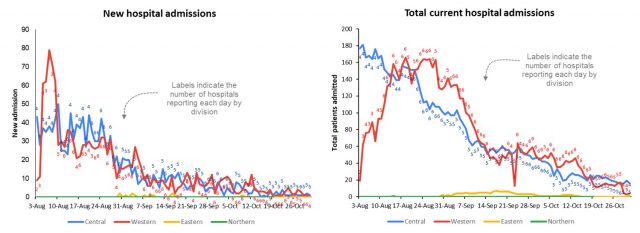
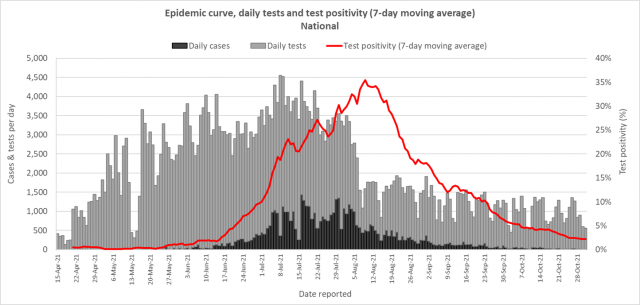
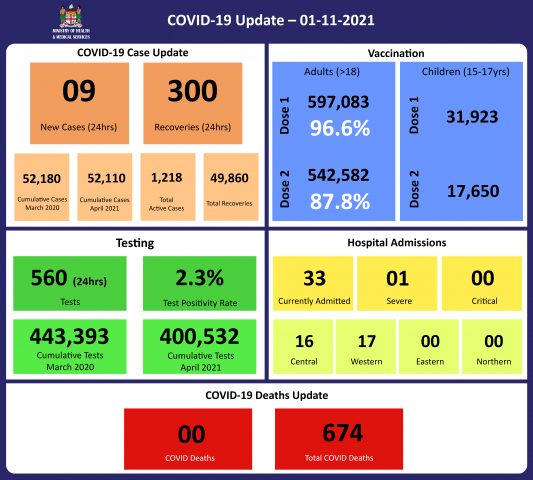
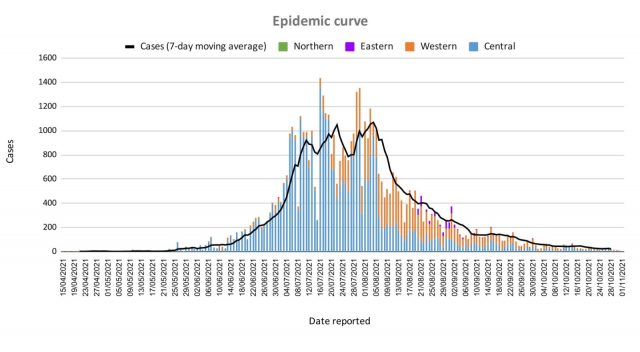
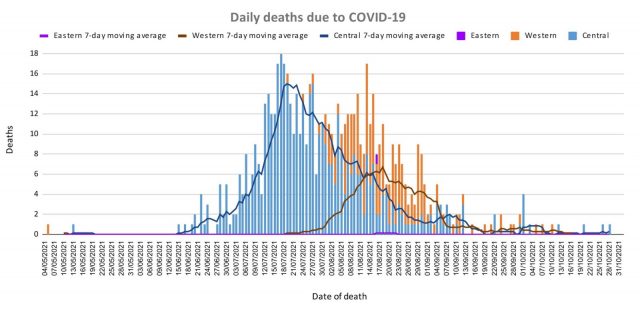
The Ministry of Health continues to monitor the outbreak using indicators such as daily case numbers, hospitalizations, test positivity, and deaths. There is a downward trend across all indicators of the COVID-19 epidemic in Fiji, indicating a positive response to our overall COVID containment and mitigation response.
Occupancy rates in health facilities, the occupancy rate of ICU beds, death rates, and vaccination coverage are indicators to monitor our health response capacity and we see a decreasing trend across indicators from our health facilities with increasing vaccination coverage for adults and 15-17-year-olds in Fiji.
Our weekly testing numbers of over 5,000 are still above the WHO recommended rate of 4 tests per 1,000 population per week (or approx. 3,500 tests per week) and we anticipate continued surveillance and testing in our communities and maritime islands to monitor and detect cases for early intervention.
Public Advisory:
A disease becomes endemic when it is expected to remain persistently present in the community. Some diseases endemic to Fiji are dengue fever and the common cold. These diseases persist at some level in the community and become epidemic when levels go beyond what is determined to be expected and acceptable.
Unfortunately, vaccine-related herd protection is not likely to be as efficient with COVID-19 as seen with some of the traditional vaccine-related diseases like measles. Recent data verified and released by the CDC indicate that unvaccinated people with the previous COVID-19 infection were 5 times more likely to have a positive COVID-19 test compared to vaccinated people. As such unvaccinated people cannot rely on herd immunity (or herd protection) nor natural immunity to protect themselves. Those eligible must get vaccinated to reduce their risk of infection, severe disease, and death. And we know vaccines are very good in preventing severe disease and deaths.
This lower efficiency in vaccine-related herd immunity also means that the public will need to live with COVID safe measures of masking, hand washing, physical distancing, and good ventilation and/or air cleaning technology. These COVID safe measures remain vital in preventing the need to go back to severely restrictive public health measures.
The Merck and Pfizer Pill
Much excitement has been generated in the media recently about the Merck Pill or Molnupiravir and the Pfizer pill.
Based on a small trial, Molnupiravir had demonstrated an up to 50% capability in reducing severe disease and death in high risk individuals when given at the onset of infection. Pfizer also reported another pill that is used with an older antiviral drug called Ritonavir. Pfizer reported a 90% reduction in severe disease and hospitalisation when used in high risk persons with mild to moderate disease. Unlike some other potential COVID treatments, either pill could be taken over five days and as part of home-based treatment. Both pills are not for use in patients with diseases severe enough to need hospital admission but seem useful for high-risk individuals, in whom home management would be seen as more ideal.
For Fiji, having access to therapeutic drugs like this would be ideal but we will need to educate people as it has to be used at the onset of mild to moderate disease when symptomatic self-care is appropriate and in settings where recognition of the severe disease is optimal. The drug will need to be so cheap and so safe that it can be used widely in the community. At the moment both drugs seem quite costly although we are aware of initiatives being taken to make Molnupiravir more affordable. There are also safety concerns that need to be well understood. We will need more details of the study itself and a peer-reviewed publication of the report is not yet widely available.
The UK medicines regulator has become the first in the world to approve Molnupiravir. The UK, like many European countries, has been focused on mitigating the risk of severe disease for tens of thousands of vulnerable patients in the upcoming winter.
In essence, both the Merck and Pfizer Pill will work well in settings where health-seeking behavior is at an optimal level. They also provide another layer of protection from severe disease and death apart from covid safe measures, avoiding contained and /or crowded spaces, ensuring good ventilation, and maintaining good vaccination. As such, the pill will need work with the other layers of protection to maximize protection from severe disease and death. To emphasize further, they do not replace any of the layers of protection measures and vaccination remains the most sustainable means to long-term protection from severe disease and death.
We are making preliminary explorations on how we can access stocks once it is more universally endorsed as they do represent a good home-based therapeutic option for high risk individuals with mild to moderate disease.
Supporting School Re-opening
COVID-19 poses a lower risk to children however secondary transmission from young school-age children can and does occur in both household and school settings. We have completed the investigation into the recent student case widely reported in the media. We can now confirm that while the student became unwell with COVID-like symptoms, his illness was not related to COVID-19. The school COVID safe protocols were well adhered to, in that he was picked up by a designated “child protection officer” in the course of oversight surveillance during the day, early notification to health authorities was done and the containment and test protocol was initiated in a timely manner.
With good vaccination coverage, high levels of COVID safe adherence, and timely instigation of measure as done in this case, it is possible for us to facilitate a measured containment program whilst continuing the school program whenever we find a positive student in school. This case and similar cases, even if truly positive, will help to refine the implementation of COVID safe measures in schools and help to put in place a quality improvement framework around the program to promote the safe opening of schools.
Students are reminded again of the need to maintain proper masking practices at all times, remain as much as possible in open ventilated spaces when with their friends, and follow all COVID safe measures especially when indoors.