Last Updated on 11 months by Publishing Team
COVID-19 Update
Thursday 15th June
| Transmission Update:
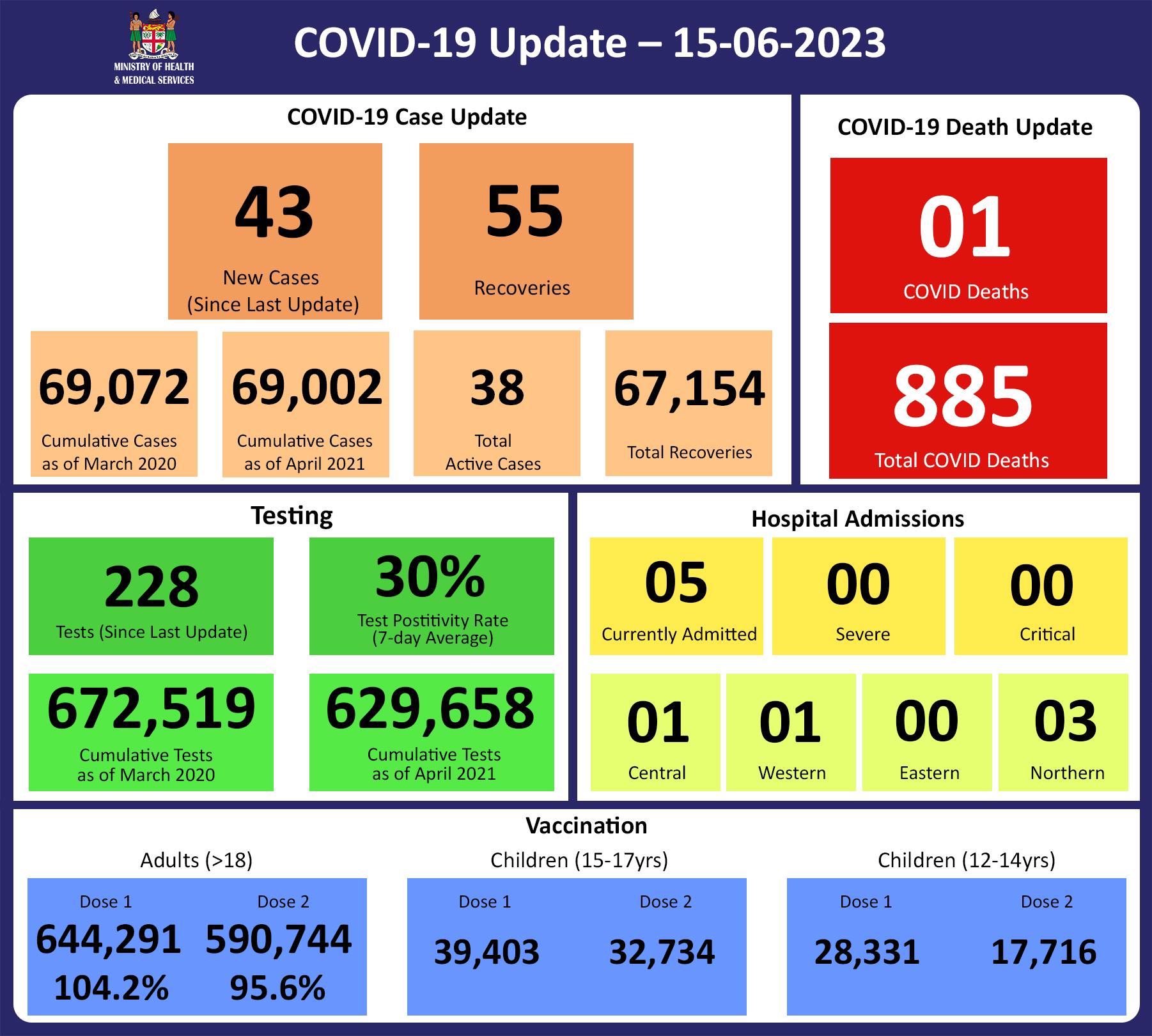
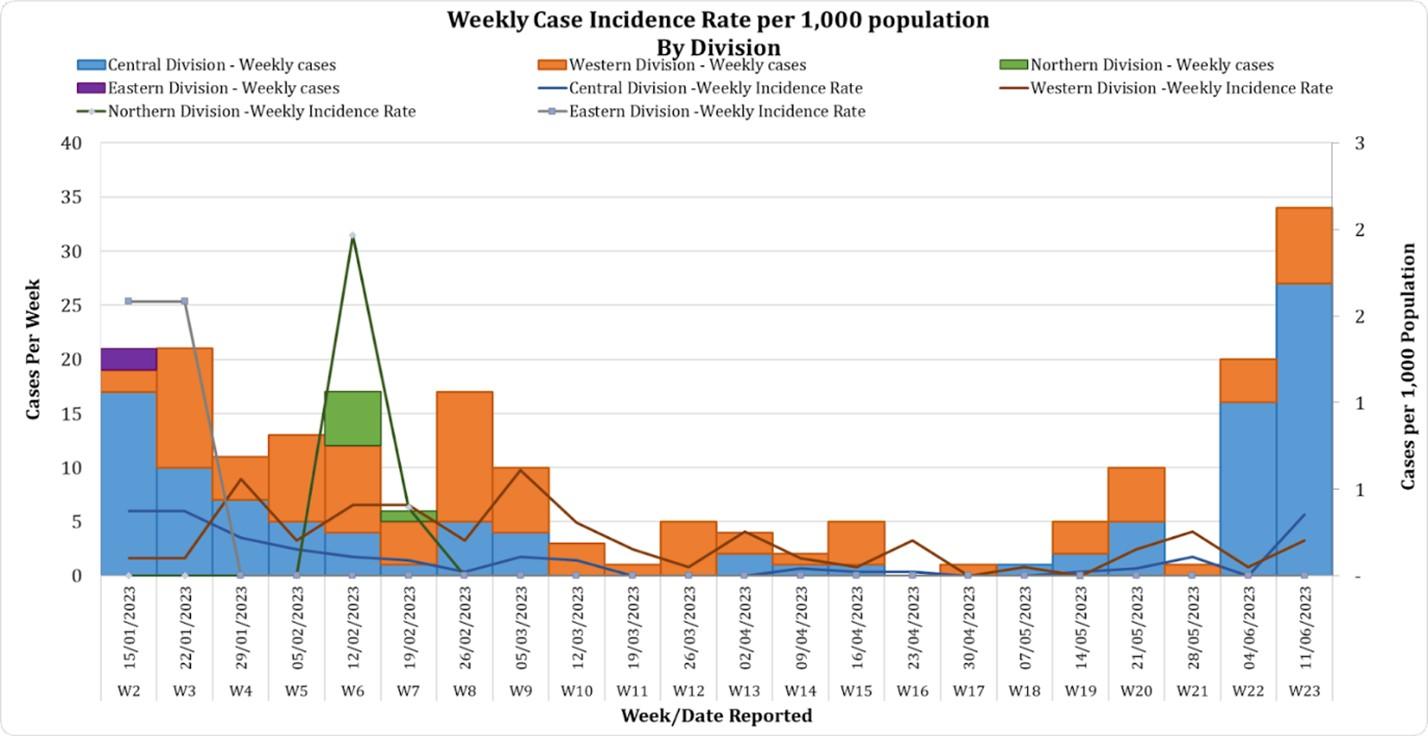
Since 08/06/23, we have recorded 49 new cases, inclusive of 6 reinfections. Of the 43 new cases recorded, 26 cases were recorded in the Central Division; 16 cases in the Western Division; 1 case in the Northern Division with nil cases in the Eastern Division. The national 7-day rolling average of cases as of 11th June is 8 daily cases. The Central Division cases constitute 66% of the cumulative total cases nationally, with the Western division making up 28%, 4% in the Northern Division, and 2% in the Eastern Division. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Deaths:
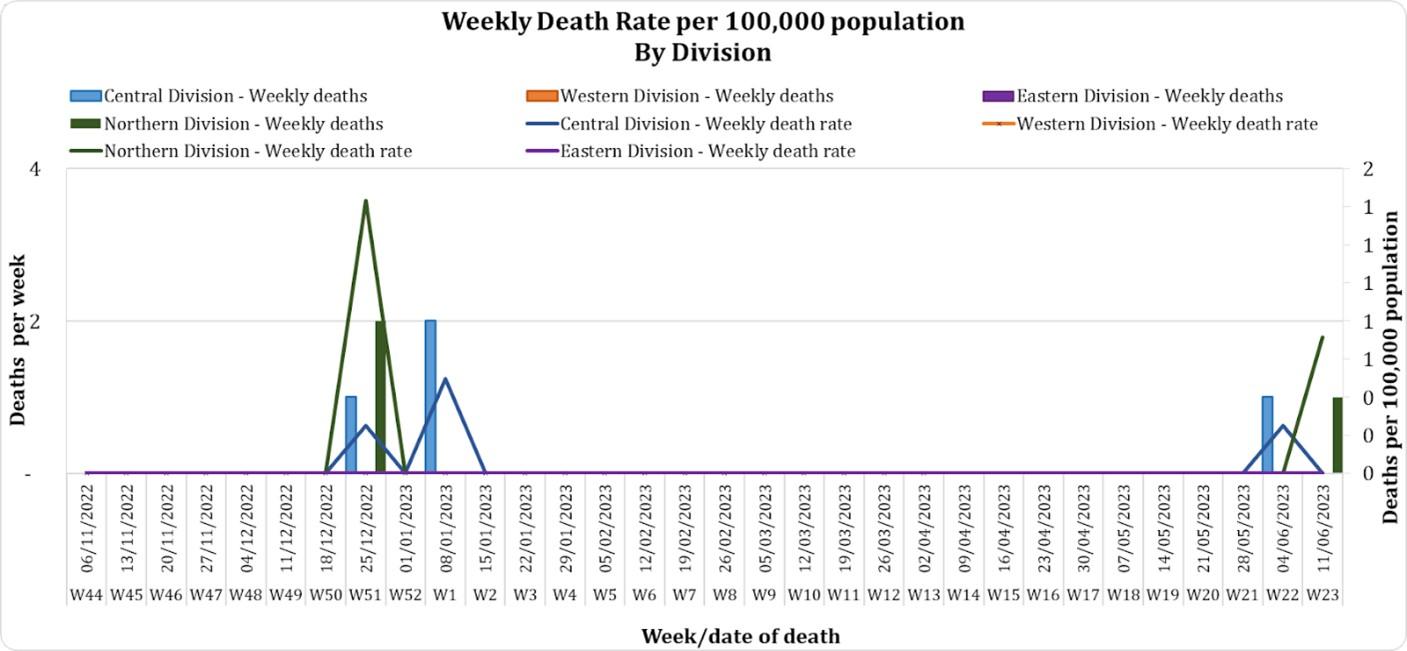
This graph depicts weekly COVID-19 deaths by division since November 2022 to current full Epi week. COVID Death Reports There is 1 COVID-19 death to report. This is a 90-year-old male from Labasa who developed respiratory symptoms on the morning of 09/06/2023. He had no pre-existing medical conditions. Sadly, he died before arrival to Labasa Hospital on 09/06/2023 from a suspected heart attack. He also tested positive for COVID-19 on 09/06/2023. He was vaccinated with 2 doses of the COVID-19 vaccine. Analysis of COVID-19 Deaths Table 1: Death rates by Division
An analysis of the 182 deaths recorded since December 2021, shows that the Central Division has the highest absolute number of deaths. The Northern Division has the highest rate of death when adjusted for population. Table 2: Deaths by Age Group
The death rate adjusted per 100,000 population, has been highest in the age group 50 years and over for the 182 deaths since December 2021. There were ten (10) deaths below the age of 19 years, 7 out of the 9 children had significant pre-existing medical conditions, and three (3) children had no known underlying medical condition. Table 3: Deaths by Vaccination Status
Of the 182 COVID-19 deaths reported since December 2021, eight (8) deaths were in the population not eligible for vaccination (under the age of 12). An analysis of the 174 deaths in the vaccine-eligible population revealed that Fiji has a death rate of 12.4 per 100,000 population for fully vaccinated adults and 344.4 per 100,000 population for unvaccinated adults. This means that unvaccinated adults in Fiji have been dying at a rate 27.8 times higher than fully vaccinated adults. Individuals in the 12-17 age group who died were not vaccinated. There has been a total of 885 deaths due to COVID-19 in Fiji. As of December 25th, 2022, the national 7 days rolling average for COVID-19 deaths per day is 0.0 with a case fatality rate of 1.28%. Due to the time required by clinical teams to investigate, classify and report deaths, a 4-day interval is given to calculate the 7 days rolling average of deaths, based on the date of death, to help ensure the data collected is complete before the average is reported. We have also recorded 1,007 COVID-19-positive patients who died from other serious medical conditions unrelated to COVID-19; their doctors have determined that COVID-19 did not contribute to their deaths, and therefore these are not classified as COVID-19 deaths. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Hospitalisation:
Currently, we do not have any (0) admissions as a direct cause of COVID-19. However, five (5) admissions have tested as covid positive but are admitted for other diseases. Patients presented to the hospital are tested before admission therefore, a high number of people who are admitted for non-covid health conditions, test positive for COVID-19 due to the current level of transmission in the community. Using the WHO clinical severity classification, there are 80% (n=4) cases in the asymptomatic and mild categories; 20% (n=1) cases in the critical category with nil cases in the moderate and severe categories. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Testing:
18 tests had been reported for 14th June 2023. The total cumulative tests since 2020 are 672,519 tests. And the 7-day daily test average is 32 tests per day or 0.0 tests per 1,000 population. The national 7-day average daily test positivity is 30%, which is above the WHO recommendation of 5%, indicating community transmission of the COVID-19 virus. |
Public Advisory
COVID-19;
There is a continuing report of new COVID-19 cases. With currently available data, the symptoms are similar to the prior strains with no evidence of more severe infection. Recent mutations of COVID-19 have led to less severe disease. This is because the virus must give up something, in this case, its ability to harm, to survive. We continue to focus on implementing COVID safe measures around those vulnerable to the severe effects of COVID-19. This includes escalating measures in hospitals, old people’s homes, and facilities catering to disabled persons. As such we expect to escalate screening protocols and masking for staff, patients, and visitors. Furthermore, visitor restrictions will be in place.
We currently enjoy a high level of protection from severe disease and as such we have supported the rescinding of all vaccine mandates. So far despite the surge in cases, the impact on hospital admission has remained manageable. There is expected to be some immune escape capability that makes the variant more transmissible. The elderly, those with chronic diseases, pregnant mothers, and children with disabilities must be closely watched. That said, the booster would still be important for people at the highest risk of getting severe disease. This includes those ages 65 and older and those who are immunocompromised. Even small, additional increases in antibody production are critically important for them.
We emphasize the point that strengthening our ability to live with COVID means we remain vigilant, maintain community-wide adoption of COVID safe measures where appropriate, and keep the impetus for immunization. This is the only means to reduce the disease spread and protect those in the community who are less able to fend for themselves.
There are several reasons it’s important to avoid getting COVID-19. Getting infected puts you at risk of severe illness, potential hospitalization, and death, especially if you are high-risk and unvaccinated.
In addition, if more people get seriously ill, it could place an unnecessary strain on an already overwhelmed hospital system. Current strains are also better at evading our immune defenses as compared to prior strains. Therefore, your risk of reinfection is higher. Getting infected also puts vulnerable populations at unnecessary risk of infection including severe illness, hospitalization, and death.
Last, you could end up with long COVID. There are currently too many unknowns regarding who is more likely to get long COVID, but the risk of developing this chronic condition after infection is very real. Millions of people have developed this and suffered for many months, including time and money lost by the inability to work.
COVID-19 is unlikely to go away completely. There are still many unknown variables. Virologists wonder whether it will behave like other coronaviruses – many of which cause the common cold. It may end up reappearing seasonally, as most of our viruses do.
In prior epidemics, viruses eventually reach a saturation threshold, meaning most of the population will be or has already been infected. At this point, when the virus has fewer people to infect, the epidemic will decrease naturally.
Hopefully, this will equate to an endemic instead of a pandemic. Endemic is a disease that is still around but at a more manageable level, without causing spikes in deaths, for example. Instead, the disease is more manageable in terms of not overwhelming the system. The hope is that if COVID-19 is not eliminated, it would become more like the common cold.
Also, anyone who falls sick should not be attending work or school, especially if they have COVID-19-like symptoms. You must get tested for COVID-19; 5-day isolation is recommended if you have tested positive.
Influenza and Acute Respiratory Illness
Our surveillance systems show that the resurgence of influenza-like and acute respiratory illnesses continues. Reports are suggesting an increase in absenteeism rates in schools and workplaces.
Earlier this year, we had an outbreak of a type of Influenza type A virus scientifically labeled as FluA/H1 Pdm. This outbreak had receded however, we now have indications of another outbreak of Flu-like illness. Essentially, we are observing a “double peak trend” (bi-phasic) of Influenza-like illness (ILI) case reports over the last several months since December 2022. As observed from past years’ trends, Fiji’s annual influenza season runs from January to May – June.
The Fiji CDC has confirmed that Influenza B/Victoria is now the predominant influenza strain in circulation, and likely the cause of this surge of ILI cases being reported and observed locally. It must be noted that this increased presence of influenza B in circulation is similarly being observed in other countries of the region and the world.
We have Tamiflu (antiviral medications) stock which is being distributed and we are getting more Flu vaccines which will be offered to those vulnerable to the severe effects of Influenza (individuals with chronic illness, pregnant women, and to frontline staff. Surveillance has also been escalated and we await more recent reports to determine ongoing trends. Whilst we still have stocks of flu testing reagents and consumables, we are also working with WHO to increase our stocks.
The Ministry of Health and Medical Services advises public members to stay at home when feeling unwell or wear face coverings (masks) when going outside to minimize the spread of infection.
We also advise that people living with chronic disease and children, especially babies, need to be protected from the severe effects of influenza. This entails preventing infection by proper masking in crowded and/or poorly ventilated spaces, early recognition of the symptoms, and seeing a doctor early. It is essential that these vulnerable persons are carefully monitored to ensure early access to intervention if severe symptoms develop.
Preventative measures will be familiar as they are similar to COVID-19. Wear a mask that covers your mouth and nose when in a public place, wash your hands frequently with soap and water or use an alcohol-based hand sanitizer, avoid crowds, stay home if you are sick, and cover your mouth and nose if you cough or sneeze.
Seek medical care: For adults, see a Doctor if the following danger symptoms develop; difficulty breathing or shortness of breath, pain or heaviness in the chest, persistent fever ( more than 3 days, despite home treatment), very high temperature (over 40°C), feeling sicker as time goes by, confusion and persistent drowsiness, severe headache that doesn’t respond to painkillers and unusual symptoms such as hallucinations, severe vomiting, neck stiffness, skin rash, rapid heart rate, chills, uncontrollable shivering, or muscle spasms.
For children, seek medical care right away if your child:
- has a fever greater than 38°C for more than two days, or a fever of 40°C or higher for any amount of time
- has a fever of 38°C or higher and is under 3 months old
- has a fever that doesn’t get better after taking Panadol
- seems unusually drowsy or lethargic
- won’t eat or drink
- is wheezing or is short of breath
COVID-19 Vaccination
While we are expecting new supplies of COVID vaccines at the end of next month (July), the Pediatric supplies of vaccines are available for children aged 5 to 11 years which is accessible at the nearest Health Center.
We have been reporting that 100% of our estimated adult population have received one dose and 95% have received the second dose. The vaccination of our target population has been progressing well with the 12 years and above coverage rate for Fiji being 99% for Dose 1 and 89% for Dose 2.
Additionally, as of the 15th of June, 172,078 (55%) booster-eligible individuals have so far received their 3rd dose while 29,929 individuals have been administered the 4th dose.
We urge the unvaccinated adults and children to get their vaccine status updated. Those who are residing in the Central and Western Division and are yet to receive their 1st and 2nd doses and especially the children in the Rewa and Nasinu schools. All travelers are also encouraged to get themselves vaccinated.
To register online for the first dose, please visit vra.digitalfiji.gov.fj
The public is reminded that vaccination sites are strictly closed at 3 pm. Therefore, any person going to the site in the afternoon is requested to be present at least by 1.30 pm.
Sites for vaccination will be operational from 9 am – 3 pm each day (Monday – Friday) while Suva Health Center will also operate on Saturdays (9 am – 3 pm).
The list of sites is available at: bit.ly/35Fozux