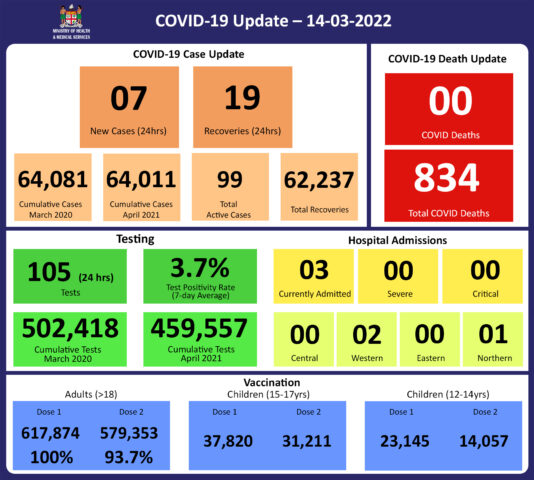
COVID-19 Update 14-03-2022
COVID-19 Update
Monday 14th March
Public Advisory:
LTDD Response update
As previously mentioned, the recent weather has resulted in conditions conducive to outbreaks of leptospirosis, typhoid, and dengue fever, which are climate-sensitive diseases endemic to Fiji. We are also aware of continued heavy rain in parts of the country, particularly the Western Division, and our experience has been that leptospirosis cases, hospitalisations, and deaths increase following similar weather events. As such the medical advice we provide needs to be followed, while we continue to mount our public health and clinical response. Please heed our advice to protect yourselves and your loved ones.
The outreach efforts in Rakiraki continue however the FEMAT support team will be wrapping up services today for a much-needed break.. Four teams consisting of one medical officer, one nurse, and one health inspector were deployed to different medical areas. Their objectives were to;
- Reach out to all the villages in the Ra sub-division within 2 weeks.
- Actively look for and treat patients with suspected LTDD.
- Create awareness for all the villages in the Ra sub-division on LTDDs.
At the end of the 2 weeks, the team was able to cover 152 communities (81 villages and 71 settlements) 100% of all villages and 76% of all settlements. The teams have been able to see a total of 1530 patients of which 132 were suspected of Leptospirosis, 10 were suspected Typhoid and 11 cases were retrieved. Of the cases, retrieved 2 were confirmed Typhoid, and 4 were confirmed Leptospirosis.
4 cases that had blood samples for testing taken in the community tested positive for leptospirosis, but had already been treated early as an outpatient by the outreach teams, and therefore prevented admissions.
Substantial reductions in admissions, severe cases needing transfer to Lautoka Hospital, and LTDD deaths from the Ra Medical Area is a well-documented impact of the FEMAT supported outreach program in Rakiraki
The typhoid fever situation in Rakiraki has also been largely contained with 7 cases from one area of which there were 3 deaths.
All close contacts of typhoid cases have been given a course of antibiotics. The area will be under surveillance for one month with regular visits to ensure the implementation of a sanitation program with improved quality of water and food hygiene practices. Screening tests will also be done to look for healthy carriers. An ongoing awareness program was supplemented today with the attendance of the Roko Tui Ra, Police, and Ra health team accompanied by the Minister for Health to bolster our ongoing active community engagement program.
The main impact of the FEMAT deployment is that we have had a bigger increase in the suspected line list for LTDD, however, home medical treatment and follow-up capability resulted in a marked reduction in admissions and no deaths within a very short time. This impact was experienced despite ongoing weather conditions. Also while the number of cases continues to occur at outbreak levels in the Rakiraki Medical Area, the exercise facilitated early treatment which resulted in decreased severity and duration of the disease in those put on the line list. Essentially our medical teams were able to seek out and find people with leptospirosis, and treat them before they developed severe disease. Or they found people with severe leptospirosis and facilitated their rapid medical evacuation for admission to the hospital.
The active pursuit of cases in communities, however, cannot be sustained over a long time, and as such active community engagement to promote better health-seeking behaviour remains the priority means of facilitating early treatment and support.
An example of this is in the Central Division: there have been over 1059 cases on the suspected leptospirosis line list, of which, over 91% were given antibiotics relatively early. And severe leptospirosis admissions to CWM hospital and recorded deaths due to leptospirosis in the Central Division have been low, despite increasing cases. This suggests that recent interventions by the Ministry, including raising awareness for our clinicians and the general public, have resulted in more people with suspected leptospirosis coming forward early to health facilities, where they are also diagnosed and treated early. We hope this trend continues and encourage members of the public to go to your nearest health centre if you have symptoms.
Prevention
The leptospirosis bacteria is spread to humans through the urine of infected animals, such as cows, pigs, rats, and dogs. To reduce your individual risk, it is important to understand that exposure to animals, soil, mud, and floodwaters during work or recreational activities increases your risk of infection.
Important prevention measures include wearing full covered footwear at all times when going outdoors, avoiding wading or swimming in flooded waters, using clean fresh water to wash up after exposure to muddy waters, and keeping all food and drinks covered and away from rats. For workplaces, practice good personal hygiene at all times, cover cuts and wounds well, and use protective equipment, especially footwear when in flooded and/or muddy areas.
We are also urging all parents and guardians to prevent children from playing in the mud or swimming in flooded rivers or creeks, and ensure that they wear shoes when outside.
Symptoms and treatment
Early treatment can decrease the severity and duration of the disease. Please seek medical care if you have recently had contact with floodwaters, mud, or animals, and develop the following symptoms: fever, muscle pain, headache. You may also have red eyes, loss of appetite, nausea/vomiting, dizziness, or feel weak.
Leptospirosis can be treated with appropriate antibiotic medications prescribed by a doctor if treatment is sought early. Danger signs for severe leptospirosis include shortness of breath, coughing blood, chest pain, yellow eyes/skin (jaundice), signs of bleeding (including unexplained bruising), decreased or increased urination, difficulty staying awake. Severe leptospirosis is life-threatening, and anyone with these symptoms must be taken to the hospital immediately.
Typhoid fever
Typhoid fever is typically found in areas that do not have access to proper toilet facilities and/or clean drinking water. We strongly encourage people who live in rural areas, informal urban areas, and any other areas where access to clean drinking water is limited, to boil all drinking water. We must all also continue to practice basic hygiene measures such as frequently washing hands with soap and water, especially after visiting the toilet and before eating or preparing food.
Dengue fever
We continue to urge everyone to get rid of potential mosquito breeding places, such as empty containers inside and outside your homes that may collect water, including discarded tires, flower vases, and pot plant bases. Protect yourself from being bitten by mosquitoes by using mosquito screens in your homes, and mosquito repellants.
COVID-19 Vaccination
As of 14th March, a total of 110,183 individuals have so far received booster doses. Members of the public are advised to obtain their booster dose after at least 5 months from their second COVID-19 vaccine dose. Moderna vaccine and Pfizer vaccines are both available for adult booster doses.
The Ministry of Health and Medical Services will continue to monitor the advisories on post-infection immunity based on quality data that is being generated globally.
Given the current stocks of Pfizer Vaccine we have we will be using Pfizer for the ongoing primary 2 dose schedule of children and adults and as the booster dose.
Supporting International Travel
- Plan to remove 3-day hotel stay for fully vaccinated travellers from Travel Partner Countries.
Since the opening of international travel borders to travel partner countries travellers coming in from Travel Partner Countries have had to undergo an in-country test in Fiji on day 2 of stay in Fiji. To support this requirement, a 3-day hotel stay was mandated to minimize the risk of non-compliance to testing and to ensure that all positive tests were appropriately responded to while the traveller was locatable. To be clear, this 3-day stay in a Care Fiji Commitment (CFC) hotel was never a quarantine. The hotel stay is in place to facilitate the testing requirement on day 2 of arrival.
We have noted that while many countries have removed all forms of traveller sequestration, the in-country testing conditions continue. As such we are supporting current efforts to have more testing sites throughout Fiji to which travellers can book for testing, without requiring a hotel stay, as part of prior approval to come into Fiji. We are working together with the Ministry of Trade and Tourism and Ministry of Economy in the final phase of approving this in-country testing for international arrivals by private entities. These private entities will ensure that the test is available and the results will be reported back to Ministry of Health officials. They will also be mandated to report any international traveller who defaults from the mandatory testing. Any traveller defaulting a test or test provider failing to report a defaulter will be subject to legal punitive measures.
- Ongoing Review of Non-Travel Partner Country Status
This ongoing effort is mediated through the Ministry of Commerce, Trade, Tourism and Transport, and the Ministry of Economy (COVID-19 Risk Mitigation Taskforce). Non-Travel Partner Status is assessed and graduated to Travel Partner status based on COVID-19 Transmission Data (cases, admission, and deaths), COVID-19 Community Surveillance data (Test per 1000, positivity rate), and ability to detect Variants (Access to genomic sequence capability). A list of Travel partner countries is available on the following link: https://www.mcttt.gov.fj/home/traveltofiji/international-travel/#b
Last Updated on 2 years by Publishing Team