COVID-19 Update 19-01-2023
COVID-19 Update
Thursday 19th January
| Transmission Update:
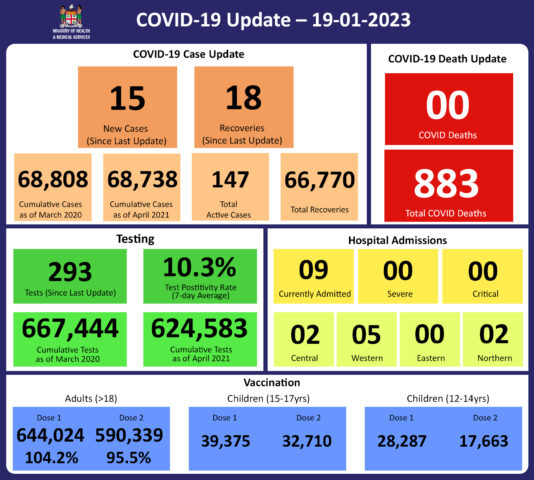
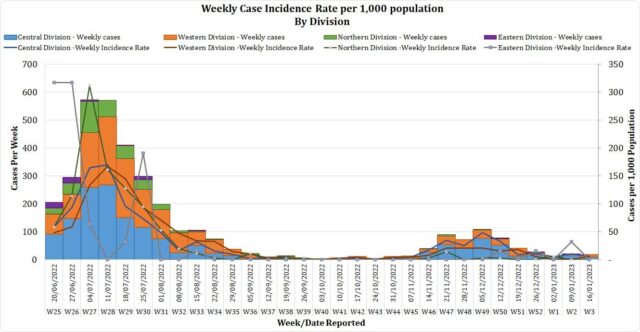
Since the last update on 12/01/23, we have recorded 15 new cases. Of the 15 new cases recorded, 9 cases were recorded in the Central Division; 6 cases in the Western Division; with nil cases in the Eastern and Northern Divisions. The national 7-day rolling average of cases as of 15th January is 3 daily cases. The Central Division cases constitute 66% of the cumulative total cases nationally, with the Western division making up 28%, 4% in the Northern Division, and 2% in the Eastern Division. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Deaths:
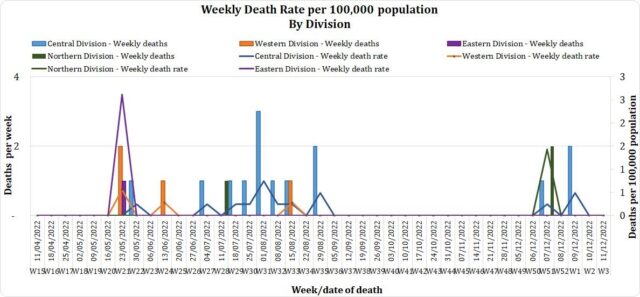
The curve depicts weekly COVID-19 deaths by division since May 2021. It indicates a surge from last December, with peaks in mid-January 2022 followed by a downward trend. COVID Death Reports We have no (0) new COVID-19 deaths to report. Analysis of COVID-19 Deaths Table 1: Death rates by Division
An analysis of the 182 deaths recorded since December 2021, shows that the Central Division has the highest absolute number of deaths. The Northern Division has the highest rate of death when adjusted for population. Table 2: Deaths by Age Group
For the 182 deaths since December 2021, the death rate adjusted per 100,000 population, has been highest in the age group 50 years and over. There were 10 deaths below the age of 19 years, 7 out of the 9 children had significant pre-existing medical conditions, and three (3) children had no known underlying medical condition. Table 3: Deaths by Vaccination Status
Of the 182 COVID-19 deaths reported since December 2021, eight (8) deaths were in the population not eligible for vaccination (under the age of 12). An analysis of the 174 deaths in the vaccine-eligible population revealed that Fiji has a death rate of 12.4 per 100,000 population for fully vaccinated adults and 344.4 per 100,000 population for unvaccinated adults. This means that unvaccinated adults in Fiji have been dying at a rate 27.8 times higher than fully vaccinated adults. Individuals in the 12-17 age group who died were not vaccinated. There has been a total of 883 deaths due to COVID-19 in Fiji. As of December 25th, 2022, the national 7 days rolling average for COVID-19 deaths per day is 0.0 with a case fatality rate of 1.28%. Due to the time required by clinical teams to investigate, classify and report deaths, a 4-day interval is given to calculate the 7 days rolling average of deaths, based on the date of death, to help ensure the data collected is complete before the average is reported. We have also recorded 1,006 COVID-19-positive patients who died from other serious medical conditions unrelated to COVID-19; their doctors have determined that COVID-19 did not contribute to their deaths, and therefore these are not classified as COVID-19 deaths. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Hospitalisation:
Currently, we do not have any (0) admissions as a direct cause of COVID-19. However, nine (9) admissions have tested as covid positive but are admitted for other diseases. Patients presented to the hospital are tested before admission therefore, a high number of people who are admitted for non-covid health conditions, test positive for COVID-19 due to the current level of transmission in the community. Using the WHO clinical severity classification, there are 78% (n=7) cases in the asymptomatic and mild categories; 11% (n=1) in the moderate category; 11% (n=1) in the severe category with nil cases in the critical category. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Testing:
57 tests had been reported for 18th January 2023. The total cumulative tests since 2020 are 667,444 tests. And the 7-day daily test average is 41 tests per day or 0.0 tests per 1,000 population. The national 7-day average daily test positivity is 10.3%, which is above the WHO recommendation of 5% and indicates the ongoing community transmission in Fiji. |
Public Advisory
For COVID-19;
As advised earlier, China is now open for inward and outward travel and given the high level of the outbreak in China and the possibility of variant formation, we are ready to review some public health border measures. At present the USA, Japan, India, South Korea, Taiwan and Australia have announced that all passengers arriving from China have a pre-departure COVID test. We currently do not have direct travel from China.
Our data indicate that we have a high level of immune protection given the low impact the current wave is having on admission capacity. The current wave in China is driven by known variants.
China and the countries that receive passengers directly from China have the ability to surveil for variants. We also have an in-country capacity now to surveil for other variants.
As such, our current stance is that no new travel restrictions will be put in place however, we also do not rule out the possibility of travel restrictions in the future.
There is a continuing trend in the increase in COVID-19 cases based on case numbers reported to us, positivity rates being compiled from hotel, airport and hospital workers and absenteeism rates from selected industries and schools. We also have registered (ten) 10 patients who have incidentally tested positive for COVID-19 while admitted to the hospital. Correspondingly, we are currently focusing on implementing COVID safe measures around those vulnerable to the severe effects of COVID-19. This includes escalating measures in hospitals, old people’s homes and facilities catering for disabled persons. As such we expect to escalate screening protocols and masking for staff, patients and visitors. Furthermore, visitor restrictions will be in place.
For the general public, we are advising that the elderly, those with chronic disease, and children with disabilities need to receive 4 doses of the vaccine and measures need to be taken to ensure they are brought to the hospital early if there is an early indication of feeling unwell, especially with respiratory symptoms. Furthermore, COVID safe measures need to be instituted around the elderly, those with chronic disease, pregnant mothers and children with disabilities. This involves proper masking of those caring for vulnerable persons, safe physical distancing for those visiting them, and ensuring they engage in highly ventilated spaces when they venture out of their homes. It is important for those with chronic diseases to be on proper treatment that ensures the optimal control of their diseases. This means that diabetics need their blood sugar to be as near normal as possible, hypertensives need their blood pressure well controlled and those with cardiac conditions to be as symptom-free as possible.
Consistent with the experience in other countries that have high vaccination rates, we anticipate a manageable impact in hospital admissions for COVID-19 disease despite increasing case numbers. While immune protection from the severe disease remains, there is expected to be some immune escape capability that makes the variant more transmissible. The elderly, those with chronic diseases, pregnant mothers and children with disabilities need to be closely watched in this regard.
We emphasise the point that strengthening our ability to live with COVID means we remain vigilant, maintain community-wide adoption of COVID safe measures where appropriate, and maintain the impetus for immunisation This is the only means to reduce the disease spread and protect those in the community who are less able to fend for themselves.
Prior to noting this increase, we had initiated the rescinding of some COVID-related public health measures relating to nightclubs, churches, sporting events and high-risk businesses. The decision to relax public health measures is based on the low number of admissions and severe cases despite the current changes in case numbers. We believe that the planned relaxation of public health measures will not have any adverse effect in terms of the number of severe COVID cases we expect to see from the recent increase in case numbers.
Also, anyone who falls sick should not be attending work or school, especially if they have COVID-19-like symptoms. You must get tested for COVID-19, and if tested positive, 7-day isolation is mandatory.
LTDD
We have noted rising trends in cases of Leptospirosis and Dengue however, our admission levels remain low and the mortality rate among admitted cases remains low. This is despite the fact that our reported case numbers had remained near or slightly above the outbreak level for most of this year. We acknowledge the efforts of our community leaders, community health workers and health workers in the primary health space for their efforts in facilitating early detection and treatment. Also, our divisional health teams with the support of the National Disaster Management Team staff have been carrying out pre-emptive source reduction measures in selected hotspots over the last month.
Recent heavy rain and flooding have affected many areas and communities throughout the country. The Ministry is focussing on geographical areas of concern for the purpose of mobilising extra capability to help manage communicable disease outbreaks and also escalate the promotion of preventative measures.
To reduce your individual risk, it is important to understand that exposure to animals, soil, mud, and floodwaters during work or recreation activities increases your risk of infection.
Important prevention measures include wearing fully covered footwear at all times when going outdoors, avoiding wading or swimming in flooded waters, using clean fresh water to wash up after exposure to muddy waters, and keeping all food and drinks covered and away from rats. For workplaces, practise good personal hygiene at all times, cover cuts and wounds well, and use protective equipment, especially footwear when in flooded and muddy areas.
Early treatment can decrease the severity and duration of the disease. Please seek medical care if you have recently had contact with floodwaters, mud, or animals, and develop the following symptoms: fever, muscle pain, and headache. You may also have red eyes, loss of appetite, nausea/vomiting, dizziness, or feel weak.
Leptospirosis can be treated with appropriate antibiotic medications prescribed by a doctor if treatment is sought early. Danger signs for severe leptospirosis include shortness of breath, coughing blood, chest pain, yellow eyes/skin (jaundice), signs of bleeding (including unexplained bruising), decreased or increased urination, and difficulty staying awake. Severe leptospirosis is life-threatening, and anyone with these symptoms must be taken to the hospital immediately.
Typhoid fever is typically found in areas that do not have access to clean drinking water. We strongly encourage people who live in rural areas, informal urban areas, and any other areas where access to clean drinking water is limited, to boil all drinking water. We must all also continue to practise basic hygiene measures such as frequently washing hands with soap and water, especially after visiting the toilet and before eating or preparing food.
COVID-19 Vaccination
We have reported that 100% of our estimated adult population have received one dose and 95% have received the second one. The vaccination of our target population has been progressing well with the 12 years and above coverage rate for Fiji being 99% for Dose 1 and 89% for Dose 2. Furthermore, as of the 19th of January, 170,632 (54.6%) booster-eligible individuals have so far received their 3rd dose while 29,085 individuals have been administered the 4th dose.
Increasing Vaccine Booster Coverage Program
We urge the public to get booster vaccine doses at the vaccination site closest to them and the list of sites is provided daily by the MHMS. Currently, both Pfizer and Moderna are recommended for booster doses.
To optimise coverage, our current target of the booster campaign is to administer 250,000 doses of the Pfizer vaccine to those who have completed the primary series (doses 1 and 2) three or more months prior but have not yet received a booster dose.
COVID-19 booster priority populations are;
- Persons over the age of 18 years who have completed their primary series > 3 months prior can receive their 1st booster dose
- Immunocompromised persons and those over the age of 60 years who had received the 3rd booster dose, may receive the 4th dose after a period of 4 months
- Healthcare workers, port staff, tourism and others who wish to receive a 2nd booster dose may receive it after an interval of 4 months from their first booster dose.
- Anyone over 18 years who have taken their 1st booster dose can receive a 2nd booster dose after an interval of 4 months.
To register online for the first dose, please visit vra.digitalfiji.gov.fj
The public is reminded that vaccination sites strictly close at 3 pm. Therefore, any person going to the site in the afternoon is requested to be present at least by 1.30 pm.
Sites for vaccination will be operational from 9 am – 3 pm each day (Monday – Friday) while Suva Health Center will also operate on Saturdays (9 am – 3 pm).
The list of sites is available at: bit.ly/35Fozux
Last Updated on 2 years by Publishing Team