COVID-19 Update 28-04-2022
COVID-19 Update
Thursday 28th April
Public Advisory
Engaging COVID safety without mandates or quarantine
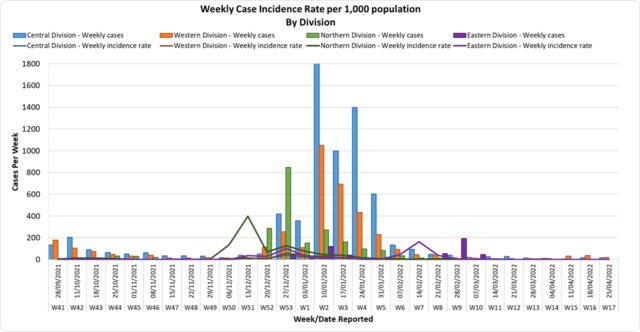
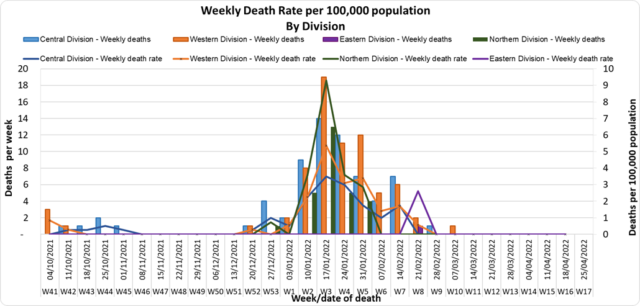
Since the 7th of April and the lifting of our quarantine measures and increased international travel, our community and border surveillance screening data continue to report a low positivity rate despite the ongoing pandemic, and the continued evolution of Omicron variants. While there is a low positivity rate among arrivals we are seeing positive arrivals. We are also aware that a key aspect of living with Covid is to have a strong community surveillance system within the community AND at the border. This will allow early identification of community outbreaks and facilitate early response. Early response capability is a key part of mitigating the risk of severe disease and severe containment measures and to further easing pre-departure conditions for international travel.
The lifting of masking and other mandates, and easing of travel restrictions is NOT a sign that the risk of outbreak and resurgence of COVID-19 is over. We reiterate the need for each individual to assess their own level of risk and decide to continue to take measures such as masking and physical distancing. For example, we know that wearing a mask in public will lower your risk of getting infected, and it is now an individual choice and responsibility that is recommended by the Ministry. If you are at higher risk of severe disease should you get infected with COVID-19, we strongly recommend that you continue to wear a mask in public, particularly in crowded indoor spaces. The promotion of COVID-safe measures will now be pursued similar to how we advise healthy lifestyle measures for the prevention of non-communicable diseases, and how basic hygiene is promoted for the prevention of infectious diseases like typhoid fever. The measures that will continue in terms of prevention are the promotion of vaccination, personal COVID-safe hygiene habits, and workplace ventilation and air cleaning measures. We recommend everyone continue to employ COVID-safe measures to prevent infection and the spread of infection: Frequently wash your hands or use an alcohol-based hand sanitiser, stay home if you feel sick, cover your mouth and nose with a tissue or the bend of your elbow if you cough or sneeze, wear a mask if you have any signs of a respiratory illness.
We also note the risk of transmission in children under 12 years, and as such we are exploring the option of requiring children under the age of 12 to also undergo pre-departure testing before travelling to Fiji. Beyond this potential change, our border protection will be mediated by the fact that travellers are vaccinated, have a negative pre-departure test, and will be tested in-country with a rapid antigen test. Currently, inbound travellers aged 12 years and above must produce proof of a pre-booked and pre-paid rapid antigen test, to be administered after 48 hours, but before 72 hours of arrival in Fiji. Booking for tests can be made through this link: https://entrytestfiji.com. There will be exemptions for those who have tested positive and recovered from COVID-19 within the 30 days before travel and have fit-to-fly certificates. Failure to comply with arrival testing once in Fiji will result in a spot fine of $1000.
Ongoing Medical Recovery Efforts
With the reduction in COVID-19 cases and in people presenting to health centres with acute respiratory illness, the MOHMS team is in a better position to focus more on health facilities and health care provision capabilities so as to mitigate against severe disease and death. This will include the ongoing community engagement and outreach program to facilitate early diagnosis and treatment in the community, and the maintenance of health facility readiness to provide treatment.
Our command centres and operation centres have been repurposed to maintain a line list of vulnerable cases in the community and to work on processes that will allow for more preemptive response and promote broader community resilience. These command centres and operation centres will also provide oversight on community surveillance indicators to ensure early and measured responses to future outbreaks.
We are also focused on carrying out general health service work more efficiently in all facilities, and a key part of our plan is to set up divisional mobile units to supplement facility-based general servicing capability and also work with private providers through a process for pre-qualifying contractors and/or suppliers for each subdivision.
The engagement of General Practitioners, Private Dental Practitioners, Private Medical Laboratories, and Private Ambulance providers to support our services in a public-private partnership arrangement is a strategy to help in our ongoing recovery efforts.
We also have reformulated a framework to better engage customer service initiatives in all health facilities and allow for senior managers to institute substantive actions and provide direct oversight over implementation plans. It will also allow the Ministry’s senior executives to track progress in implementation and ensure that annual operation plans reflect an evolving and progressive change narrative in the successive plans. These initiatives will also include the processing of internal communications to facilitate timely decision making and action within the Ministry.
COVID-19 Vaccination
As of the 28th of April, a total of 123,565 individuals have so far received booster doses. The booster dose interval for eligible persons has been reduced to 3 months from the 2nd dose. This is in recognition of the risk of disease surge based on waning 2 doses covid vaccine protection, slow booster uptake, increased international travel with the relaxation of border measures, and ongoing outbreaks in various parts of the world. Moderna vaccine and Pfizer vaccines are both available for adult booster doses.
The public is urged to get booster vaccine doses, and the list of vaccination sites is provided daily on the MOHMS social media pages as well as the website. We have accepted an offer of 50,000 doses of Pfizer paediatric doses for children aged 5 to 11 by the Aotearoa New Zealand Government. Our vaccination team is currently discussing with counterparts in NZ on further details while our efforts to source more through our other development partners are ongoing.
Our school vaccination program has also been progressing such that with the 94% adult coverage rate, 88% of all persons over 12 years have had 2 doses of the COVID 19 vaccine.
We will continue to monitor the evidence on post-infection immunity based on quality data that is being generated globally. However, until we have a better sense of the role of post-infection immunity, the Ministry of Health will continue to define our level of protection based on vaccination numbers
Given the current stocks of Pfizer vaccine we have we are using the Pfizer vaccine for the ongoing primary 2 dose schedule for children and adults, and as the booster dose.
Multi-country acute hepatitis of unknown origin
The Ministry of Health and Medical Services has been monitoring reports of acute hepatitis (liver inflammation) of unknown origin in children in multiple countries including the United Kingdom, the United States of America, Spain, Israel and France. According to the World Health Organisation, there have been 169 cases as of April 21st in 11 countries. We understand that studies into the cause of this illness in children are ongoing, and we continue to monitor reports by the World Health Organisation and other country health authorities as the investigation progresses. We have alerted our specialist children’s doctors within the Ministry, and to date, we have had no reports of cases in Fiji.
Last Updated on 2 years by Publishing Team