COVID-19 Update 30-05-2022
COVID-19 Update
Monday 30th May
Public Advisory
COVID-19 trends
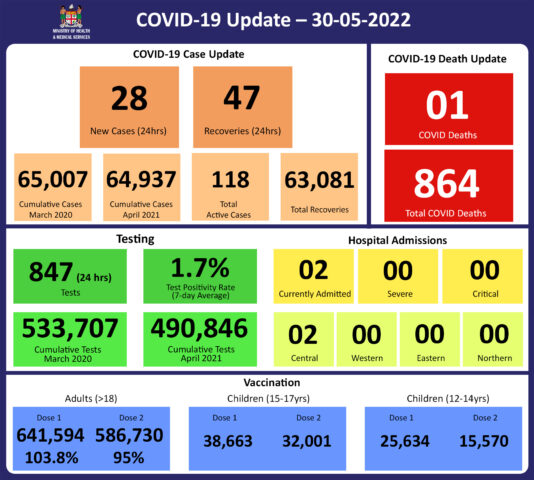
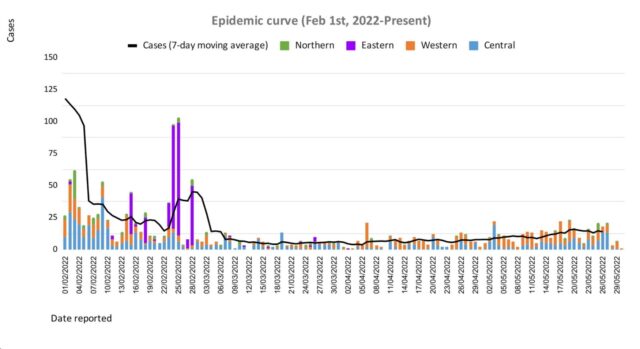
We have noted an increasing trend in cases. While the increase is not obvious on our epidemiological curve, we are maintaining close surveillance of case numbers, monitoring hospital admissions and testing for COVID-19. As indicated above while our admissions for COVID-19 remain low, this is an indicator that remains important to our ongoing response plans.
Over the recent 6 weeks, we had 461 positive cases, of which 175 were local cases and not related to travel. Among these local cases, 42% (74 cases) were unvaccinated and none had received a booster dose
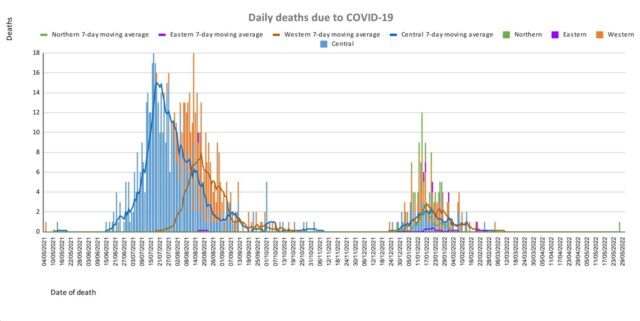
There is a second COVID-19 death recorded within a few days of the one previously reported. This case also was elderly with significant comorbidities. As we have previously mentioned, older people especially those with significant comorbidities may not mount to sufficient immune response with a 2 dose regime. In fact, the 2 reported COVID-19 deaths fall into the category that WHO recommends for booster doses.
The rise in case trends and reported deaths serve to highlight the need for greater booster dose coverage. In fact, it is in recognition of the need for increased protection of frontliners and vulnerable persons, that we now are embarking on a targeted deployment program for 2nd booster doses.
These trends are also the reason why we remain strict with the number of visitors to hospitals. We need to reduce the risk of crowding, especially during visiting hours. The vulnerable amongst us need to be protected, especially if admitted to the hospital.
International communicable disease outbreaks
AS previously mentioned, the Ministry’s Fiji Centre for Disease Control (Fiji CDC) and Border Health Protection Unit (BHPU) are monitoring international outbreaks of concern, which include Ebola Virus Disease in the Democratic Republic of Congo, Japanese Encephalitis in Australia, acute hepatitis of unknown origin in multiple countries, and monkeypox in the United Kingdom and other countries. Where appropriate, specific interventions have been put in place or strengthened in response. The situation will continue to be monitored, assessed, and responded to based on the available scientific evidence, best practice, and advice from expert authorities.
Monkeypox
As we continue our recovery path during this pandemic, the strategies for resilience require urgent and early preparedness and response planning against any potential threat.
Monkeypox is a rare disease that is caused by infection with the monkeypox virus. It is endemic to certain countries in Central and Western Africa, and the causative virus is of the same family as the smallpox virus. Monkeypox outbreaks have been recently reported in a growing number of countries that are not endemic to the disease, including the United Kingdom, Spain, Portugal, France, Italy, Germany, Sweden, the Netherlands Canada, the United States of America, and Australia.
Monkeypox is usually a self-limiting illness, which means that most people recover with just supportive treatment within several weeks. However, severe illness can occur in some individuals. It does not spread easily between people but person to person transmission may occur through:
- contact with clothing or linens (such as bedding or towels) used by an infected person
- direct contact with monkeypox skin lesions or scabs
- exposure to respiratory droplets eg coughing or sneezing
The Ministry is working with communications and community engagement teams on appropriate public advisories. We need to arm ourselves with the knowledge to protect ourselves from reducing the chances of spread in our community. Infection prevention protocols are currently being put together at the border and in community facilities. One key focus will be to ensure we have the ability to maintain oversight over travellers from selected countries to ensure early diagnosis, treatment, and contact tracing.
Overall symptoms of the virus can include:
- fever, chills, muscle aches, backache, swollen lymph nodes, and exhaustion
- an unusual rash, which typically starts on the face, and then may spread elsewhere on the body.
All doctors and Nurses in the community need to ensure they are well informed of how cases present and be vigilant in helping to ensure cases are diagnosed early.
Prevention of transmission of infection by respiratory and contact routes is required. Appropriate respiratory isolation is essential for suspected and confirmed cases. Scabs are also infectious and care must be taken to avoid infection by handling bedding, clothing, and so on. Workplaces especially in key sectors will be asked to escalate their Infection Prevention and Control and ensure practices are maintained.
The major priority for the Ministry of Health and Medical Services is to have a response plan that will include surveillance with rapid response and containment protocols and at the same time have a minimal social and economic impact. A key focus will be on ensuring that those suspected or confirmed to have monkeypox must be able to be managed in a dignified manner with no threat of stigmatisation. Each citizen’s duty to contribute to protecting Fiji must be the priority.
We are in discussions with our reference laboratory in Melbourne to ensure access to definitive tests. Our ongoing efforts to have genomic sequencing capability in the Fiji CDC will provide us with greater capacity to deal with infection threats now and in the future.
We are also in discussions with WHO to ensure we preposition access to vaccines and medications used to treat monkeypox.
However, it is important to ensure that in escalating community-wide infection prevention and control measures, we are responding to current threats and creating community-wide resilience to upcoming threats. Our ongoing engagement in a healthy lifestyle to mitigate NCDs is also part of the overall focus on building back better and stronger.
The Ministry of Health and Medical Services will be disseminating more specific advisories over the next few days to weeks. Further updated knowledge about the monkeypox virus will be shared as they are known.
Ongoing Medical Recovery Efforts
With the reduction in COVID-19 cases and in people presenting to health centres with acute respiratory illness, the MOHMS team is better positioned to focus more on health facilities and health care provision capabilities to mitigate against severe disease and death. This will include the ongoing community engagement and outreach program to facilitate early diagnosis and treatment in the community, and the maintenance of health facility readiness to provide treatment.
Our command centres and operation centres have been repurposed to maintain a line list of vulnerable cases in the community and to work on processes that will allow for more preemptive response and promote broader community resilience. These command centres and operation centres will also provide oversight on community surveillance indicators to ensure early and measured responses to future outbreaks.
We are also focused on carrying out general health service work more efficiently in all facilities, and a key part of our plan is to set up divisional mobile units to supplement facility-based general servicing capability and also work with private providers through a process for pre-qualifying contractors and/or suppliers for each subdivision.
The engagement of General Practitioners, Private Dental Practitioners, Private Medical Laboratories, and Private Ambulance providers to support our services in a public-private partnership arrangement is a strategy to help in our ongoing recovery efforts.
We also have reformulated a framework to better engage customer service initiatives in all health facilities and allow for senior managers to institute substantive actions and provide direct oversight over implementation plans. It will also allow the Ministry’s senior executives to track progress in implementation and ensure that annual operation plans reflect an evolving and progressive change narrative in the successive plans. These initiatives will also include the processing of internal communications to facilitate timely decision making and action within the Ministry.
COVID-19 Vaccination
As of the 30th of May, a total of 129,510 individuals have so far received booster doses. This represents 29.5% of those eligible for a booster dose. The booster dose interval for eligible persons has been reduced to 3 months from the 2nd dose. This is in recognition of the risk of disease surge based on waning 2 doses covid vaccine protection, slow booster uptake, increased international travel with the relaxation of border measures, and ongoing outbreaks in various parts of the world. Moderna vaccine and Pfizer vaccines are both available for adult booster doses.
Since Friday, 27th of May we began administering the second COVID-19 booster dose to the eligible population who are aged 18 years and above. They can get the second booster after an interval of 4 months from receiving their first booster dose.
The public is urged to get booster vaccine doses, and the list of vaccination sites is provided daily on the MOH. We have accepted an offer of 50,000 doses of Pfizer paediatric doses for children aged 5 to 11 by the Aotearoa New Zealand Government. Our vaccination team is currently discussing with counterparts in NZ on further details while our efforts to source more through our other development partners are ongoing.
Our school vaccination program has also been progressing such that with the 95% adult coverage rate, 90.6% of all persons over 12 years have had 2 doses of the COVID-19 vaccine.
We will continue to monitor the evidence on post-infection immunity based on quality data generated globally. However, until we have a better sense of the role of post-infection immunity, the Ministry of Health will continue to define our level of protection based on vaccination numbers
Given the current stocks of Pfizer vaccines, we are now covering the Primary doses for those yet to be vaccinated and for Dose 2 if individuals were vaccinated with either Moderna or Astra Zeneca while the 12-14-year-olds continue with the Pfizer vaccine.
Cold and flu
The Ministry of Health and Medical Services has noted an increase in people becoming ill with cold and flu-like illnesses as we are coming into our dry and cold season. This increase is especially seen in infants and children under the age of 5. The paediatrics department at CWM Hospital is also seeing an increase in children under the age of 5, especially infants, being admitted with acute respiratory illnesses while testing negative for COVID-19 and influenza. It has been expected that as restrictions intended to prevent transmission of COVID-19 were lifted (including mandatory masking, physical distancing, and school and border closures) other respiratory viruses that normally circulate would begin to re-emerge similar to pre-COVID levels, and possibly even at higher levels due to a decrease in population immunity to seasonal viruses, as cold/flu cases were low during the last two years.
Last Updated on 2 years by Publishing Team