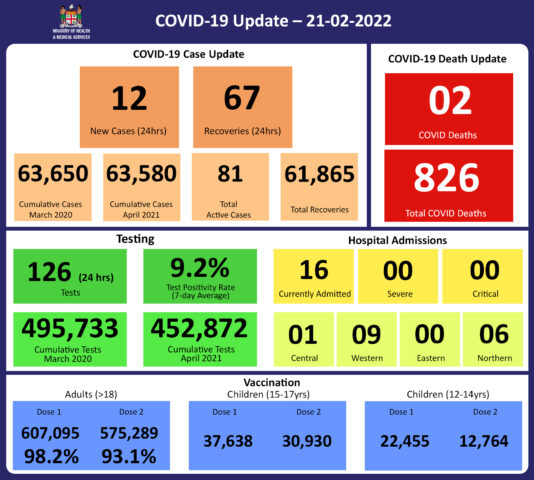
COVID-19 Update 21-02-2022
COVID-19 Situation Update
Monday 21st February
Public Advisory:
Leptospirosis, typhoid fever, and dengue fever
We have an outbreak of leptospirosis in the West and the Central Division, an increasing trend of leptospirosis in the North, and dengue fever in the Western Division. These are both climate-sensitive diseases that are endemic to Fiji.
For leptospirosis, most of the cases are in the West, with Lautoka hospital recording a total of 63 hospital admissions. Of these admissions, 39 cases were admitted to Sub-Divisional Hospitals and 24 cases in Lautoka hospital. Even more concerning is that we had 12 admissions to Lautoka hospital over the weekend of which 9 were admissions to the Intensive Care Unit. We also have a smaller leptospirosis outbreak in the Central Division with 4 admissions to the hospital and none of these current admissions needing ICU care. Labasa hospital has currently had 9 admissions for leptospirosis.
There have been 5 more leptospirosis deaths since the last update on February 16th, with 4 deaths in the West (from Bukuya, Tavua, and Rakiraki) and 1 in the Northern Division (from Macuata). 3 of the people who died were in their 20s; 1 was in their 30s; 1 was in their 50s. This brings to a total of 19 deaths nationally, with 16 deaths in the West, 1 in the Central Division, and 2 in the North this year.
As previously reported, delay in accessing care has been noted to contribute significantly to these adverse outcomes.
The clinical and epidemiological data indicate that males and young adults aged 20-49 years high-risk groups, and young iTaukei males are overly represented in cases and severe outcomes. The disease however can however infect anyone as the risk is mediated by greater occupational and recreational exposure to animals, soil, mud, and water. Of particular note is the playing of sports on muddy flood-affected grounds. Other risk factors include farming, working outdoors or in abattoirs; living in households that have rats living nearby; raising pigs at home, or the presence of pigs in the community.
Members of the public must understand that to prevent leptospirosis, one should avoid wading or swimming in flooded waters, wear shoes when outside, and keep all food and drinks covered and away from rats. For workplaces the importance of controlling pests, practising good personal hygiene, using protective equipment, especially footwear when in flooded and/or muddy areas.
Early treatment can decrease the severity and duration of the disease. Please seek medical care if you have recently had contact with floodwaters, mud, or animals, and develop the following symptoms: fever, muscle pain, headache. You may also have red eyes, loss of appetite, nausea/vomiting, dizziness, or feel weak. Leptospirosis can be treated with appropriate antibiotic medications prescribed by a doctor if treatment is sought early. Danger signs for severe leptospirosis include shortness of breath, coughing blood, chest pain, yellow eyes/skin (jaundice), signs of bleeding (including unexplained bruising), decreased or increased urination, difficulty staying awake. Severe leptospirosis is life-threatening, and anyone with these symptoms must be taken to the hospital immediately.
For typhoid fever, we have seen case numbers less than expected for the current period. We are hopeful that this is the impact of the WASH (Water, Sanitation and Hygiene) initiative that had been ongoing since tropical cyclone Yasa and Ana. Typhoid fever is typically found in areas that do not have access to clean drinking water such as rural areas and urban informal settlements. We strongly encourage people, especially those in rural areas, informal urban areas, and any other areas where access to clean drinking water is limited, to boil all drinking water. We must all also continue to practice basic hygiene measures such as frequently washing hands with soap and water, but especially after visiting the toilet and before eating or preparing food.
Dengue cases are also within expected numbers however recent increases in cases do represent a serious concern. We continue to urge everyone to get rid of potential mosquito breeding places, such as empty containers outside your homes that may collect water, including discarded tires. You must also prevent yourself from being bitten by mosquitoes through the use of mosquito screens in your homes, and mosquito repellants.
Our outreach team to Navosa is currently wrapping up operations this week. The team was able to facilitate access into poorly accessible areas affected by floods and designated as red zones. Suspected cases were counselled on ongoing care and sick ones were transferred to the hospital to receive the appropriate treatment. They were also able to review chronic medical cases and update their management. COVID immunisation and booster together with catch-up immunisation was run as a parallel program together with a Social Welfare support program. Environmental Health Officers were also brought in to assist with coverage of the areas of need.
Vaccination
We have completed our current stocks of Astrazeneca and we will get more stocks in the next 6 weeks. We will continue to deploy Moderna and Pfizer as primary doses for children and adults, and booster doses for adults.
The booster dose program began at the end of November 2021. As of the 21st of February, 97215 individuals have so far received booster doses.
Many questions have been received on the role of post-infection immunity in defining our COVID-protected population. Then immunity gained through a vaccination program remains the only means by which we can measure immunity and therefore refine public health measures in the face of the ongoing risk of variant development and therefore future outbreaks. The Ministry of Health and Medical Services will continue to monitor the advisories on post-infection immunity based on quality data that is being generated globally
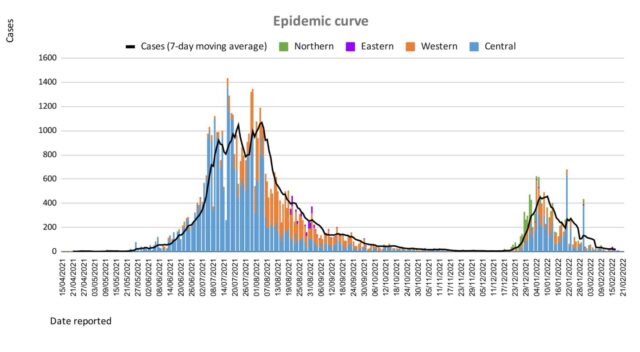
Living with COVID 19
We need to be wary of efforts to remove all public health measures too soon. Globally there are ongoing risks of variant development and therefore the escalation of the epidemic in Fiji. Building a national resilience to living with COVID 19 is crucial. This requires 2 important strategies from a health program perspective.
1. More balanced use of public health measures.
Hand washing and cough etiquette are immovable as public health measures. Regular hand sanitization and coughing/sneezing into a tissue or handkerchief, or the bend of your elbow, are healthy habits that protect yourself and others from COVID-19 and other infectious diseases. Isolating yourself, or staying away from others, when you are sick with any respiratory illness is also a good habit to protect others, especially the vulnerable.
Masking, physical distancing, and ventilation are 3 measures that must constantly be present, but there is some flexibility in increasing 2 others when one of the measures becomes difficult to apply. Whatever the scenario, an effective mask must be kept close to you at all times. The current masking requirement that wearing a mask that covers your nose and mouth is mandatory in all public places for everyone aged 8 and over, including in public service vehicles remains in force. The Ministry of Health and Medical Services is looking into a list of exemption criteria; however, we expect that this list will not be exhaustive and we hope to leave some space for a common-sense approach to evolve.
In a setting where physical distancing of 2 metres is more difficult, then increasing ventilation and more strict masking practice will be needed even more. A well-ventilated indoor space refers to an indoor space wherein there is a good movement of outside air coming into the space, and inside air is going out. A suboptimally ventilated space is bad for many reasons aside from COVID, however, in this scenario, the physical distancing rules will increase and masking is more necessary. For custodians of workplaces, houses of worship, and the like, balancing the relationship between ventilation, physical distance, and masking is the only way to ensure that services are COVID safe and can be customised to the principle of living with the virus. SOPs need to be configured to all activities that occur in your work or worship space in order to be COVID Safe resilient. We all want to mitigate the risk of unsustainable sick leave levels every time we get a variant, and more variants will come. Mitigating the risk of people getting sick is the best way to reduce further the risk of severe disease and death beyond the protection afforded by vaccination. Promoting good COVID safe principles in a common-sense approach is the best way to start.
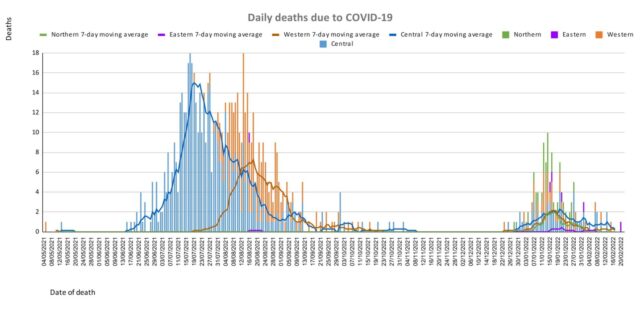
2. Protecting the Vulnerable
We have highlighted how severe comorbidities and poor health-seeking behaviour have vastly contributed to severe outcomes in the COVID outbreak. We need to build resilience in the face of an endemic problem. Based on the lessons learned from the deaths, we need to:
- Prevent all preventable chronic diseases of which NCDs are the most prominent
- Promote the better control of controllable chronic diseases of which NCDs are the most prominent, and
- Build stronger support for better health-seeking behaviour, especially among the vulnerable amongst us
We are urgently reviewing and strengthening our public health measures to find, stop and prevent health threats wherever they arise. Our sub-divisional health teams have been reminded to review and strengthen their community surveillance program and line list management of vulnerable persons.
However, the impact of these efforts cannot be sustained unless we get a broad level of support from the community in implementing the above 3 strategies, and at the same time reducing the transmission of COVID-19 to protect our vulnerable populations. Maintaining the Vaccine Plus approach remains critical.
Last Updated on 2 years by Publishing Team