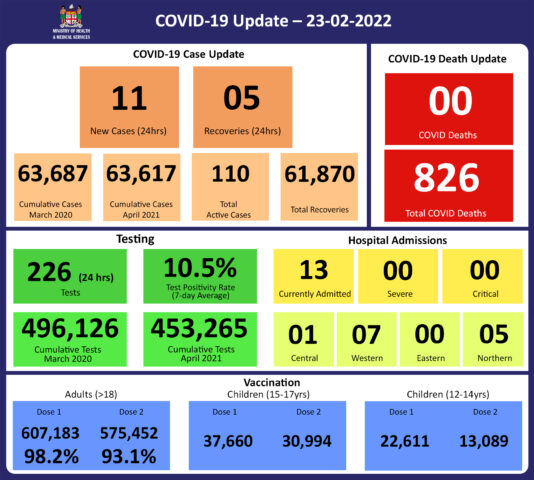
COVID-19 Update 23-02-2022
COVID-19 Situation Update
Wednesday 23rd February
Public Advisory:
Leptospirosis, typhoid fever, and dengue fever
The outbreak of leptospirosis in the Western Division continues, with 162 test positive cases recorded so far this year. There have also been 110 cases in Central, 67 in the North, and 8 cases in the Eastern Division. Cases have been predominantly in the 1 – 39-year-old age group, 61% male and 39% female, and 79% in the i-Taukei population.
The increasing hospitalisations and deaths caused by leptospirosis in the Western Division are of great concern. There have been 108 leptospirosis admissions in the West this year. An increasing trend is noted, with 17 cases two weeks ago, and 42 admissions last week. 27 hospital admissions have been reported at Rakiraki hospital, with 19 of these admissions in the last week. Ba hospital has recorded 19 admissions, with 5 in the last week. Nadroga/Navosa subdivision has had 14 hospital admissions, with 5 in the last week. Nadi hospital reported 9 admissions, with 5 in the last week. And Tavua subdivision with 5 hospital admissions, including 4 in the last week. There have been 52 leptospirosis admissions to Lautoka hospital, including transfers of patients admitted at the above-mentioned subdivisional hospitals.
Sadly, 17 people have died of leptospirosis in the Western Division this year, with 1 more death since the last update on 21/02/22.
Our outreach team to Navosa is currently wrapping up operations this week following a successful campaign in the Navosa medical area. The new area of concern is the Ra Medical area where we have noted a marked increase in cases and hospitalisations. We will be mobilizing support to the Ra Subdivision Medical Team to meet the escalated need of accessing hard-to-reach communities affected by recent floods and designated as red zones. Suspected cases will be counselled on ongoing care and the severely ill will be transferred to the hospital to receive the appropriate treatment. The team will also be able to review chronic medical cases and update their management. COVID immunisation and booster doses together with the catch-up immunisation campaign for children will run as a parallel program, together with a Social Welfare support program. Environmental Health Officers have also been brought in to work with the community in escalating cleanup efforts that help to control the population of communicable disease vectors such as mosquitoes, rats, and other rodents in affected areas. Community engagement efforts are also in place measures to educate the community on the risk of exposure to floodwaters and to discourage our people from playing in flooded areas and muddy places that increase their risk of contracting leptospirosis and other water-borne diseases.
There has been a public request that the Ministry of Health should provide a breakdown of which areas in the division are considered red zones for these climate-sensitive diseases so as to help people be on the lookout especially if they are planning to visit certain communities. We need to be clear that the floods have affected all areas of the west. We are looking at geographical areas of concern for the purpose of mobilizing extra capability to help manage the outbreak and also escalate the promotion of preventative measures. To reduce your individual risk, it is important to understand that the risk to humans is mediated by greater occupational and recreational exposure to animals, soil, mud, and water.
Important prevention measures include wearing full covered footwear at all times when going outdoors, avoiding wading or swimming in flooded waters, regular use of clean fresh water to clean up, especially after exposure risk in flooded and/or muddy areas, and keeping all food and drinks covered and away from rats. For workplaces the importance of controlling pests, practicing good personal hygiene, using protective equipment, especially footwear when in flooded and/or muddy areas.
Early treatment can decrease the severity and duration of the disease. Please seek medical care if you have recently had contact with floodwaters, mud, or animals, and develop the following symptoms: fever, muscle pain, headache. You may also have red eyes, loss of appetite, nausea/vomiting, dizziness, or feel weak. Leptospirosis can be treated with appropriate antibiotic medications prescribed by a doctor if treatment is sought early. Danger signs for severe leptospirosis include shortness of breath, coughing blood, chest pain, yellow eyes/skin (jaundice), signs of bleeding (including unexplained bruising), decreased or increased urination, difficulty staying awake. Severe leptospirosis is life-threatening, and anyone with these symptoms must be taken to the hospital immediately.
For typhoid fever, we have seen case numbers less than expected for the current period. We are hopeful that this is the impact of the WASH (Water, Sanitation and Hygiene) initiative that has been ongoing since tropical cyclone Yasa and Ana. Typhoid fever is typically found in areas that do not have access to clean drinking water such as rural areas and urban informal settlements. We strongly encourage people, especially those in rural areas, informal urban areas, and any other areas where access to clean drinking water is limited, to boil all drinking water. We must all also continue to practise basic hygiene measures such as frequently washing hands with soap and water, but especially after visiting the toilet and before eating or preparing food.
Dengue cases are also within expected numbers however recent increases in cases do represent a serious concern. We continue to urge everyone to get rid of potential mosquito breeding places, such as empty containers outside your homes that may collect water, including discarded tires. You must also prevent yourself from being bitten by mosquitoes through the use of mosquito screens in your homes, and mosquito repellants.
Vaccination
We have completed our current stocks of AstraZeneca and we will get more stocks in the next 6 weeks. Meanwhile, we will continue to deploy Moderna and Pfizer as primary doses for children and adults, and booster doses for adults.
The booster dose program began at the end of November 2021. As of the 23rd of February, 98,683 individuals have so far received booster doses.
Many questions have been received on the role of post-infection immunity in defining our COVID-protected population. Then immunity gained through vaccination remains the only means by which we can measure immunity and therefore refine public health measures in the face of the ongoing risk of variant development and therefore future outbreaks. The Ministry of Health and Medical Services will continue to monitor the advisories on post-infection immunity based on quality data that is being generated globally
Living with COVID 19
We should be wary of efforts to remove all public health measures too soon. Globally, there are ongoing risks of variant development and therefore the escalation of the epidemic in Fiji. Building the national resilience to living with COVID 19 is crucial. This requires 2 important strategies from a health program perspective.
1. More balanced use of public health measures.
Hand washing and cough etiquette are immovable as public health measures. Regular hand sanitization and coughing/sneezing into a tissue or handkerchief, or the bend of your elbow, are healthy habits that protect yourself and others from COVID-19 and other infectious diseases. Isolating yourself, or staying away from others, when you are sick with any respiratory illness is also a good habit to protect others, especially the vulnerable.
Masking, physical distancing, and ventilation are 3 measures that must constantly be present, but there is some flexibility in increasing 2 others when one of the measures becomes difficult to apply. Whatever the scenario, an effective mask must be kept close to you at all times. The current masking requirement that wearing a mask that covers your nose and mouth is mandatory in all public places for everyone aged 8 and over, including in public service vehicles remains in force. The Ministry of Health and Medical Services is looking into a list of exemption criteria; however, we expect that this list will not be exhaustive and we hope to leave some space for a common-sense approach to evolve.
In a setting where physical distancing of 2 metres is more difficult, then increasing ventilation and more strict masking practice will be needed even more. A well-ventilated indoor space refers to an indoor space wherein there is a good movement of outside air coming into the space, and inside air is going out. A suboptimally ventilated space is bad for many reasons aside from COVID, however, in this scenario, the physical distancing rules will increase and masking is more necessary. For custodians of workplaces, houses of worship, and the like, balancing the relationship between ventilation, physical distance, and masking is the only way to ensure that services are COVID safe and can be customized to the principle of living with the virus. SOPs need to be configured to all activities that occur in your work or worship space in order to be COVID Safe resilient. We all want to mitigate the risk of unsustainable sick leave levels every time we get a variant, and more variants will come. Mitigating the risk of people getting sick is the best way to reduce further the risk of severe disease and death beyond the protection afforded by vaccination. Promoting good COVID safe principles in a common-sense approach is the best way to start.
2. Protecting the Vulnerable
We have highlighted how severe comorbidities and poor health-seeking behaviour have vastly contributed to severe outcomes in the COVID outbreak. We need to build resilience in the face of an endemic problem. Based on the lessons learned from the deaths, we need to:
- Prevent all preventable chronic diseases of which NCDs are the most prominent
- Promote the better control of controllable chronic diseases of which NCDs are the most prominent, and
- Build stronger support for better health-seeking behaviour, especially among the vulnerable amongst us
We are urgently reviewing and strengthening our public health measures to find, stop and prevent health threats wherever they arise. Our sub-divisional health teams have been reminded to review and strengthen their community surveillance program and line list management of vulnerable persons.
However, the impact of these efforts cannot be sustained unless we get a broad level of support from the community in implementing the above 3 strategies, and at the same time reducing the transmission of COVID-19 to protect our vulnerable populations. Maintaining the Vaccine Plus approach remains critical.
Last Updated on 2 years by Publishing Team