Last Updated on 2 years by Publishing Team
Epidemic Outlook:
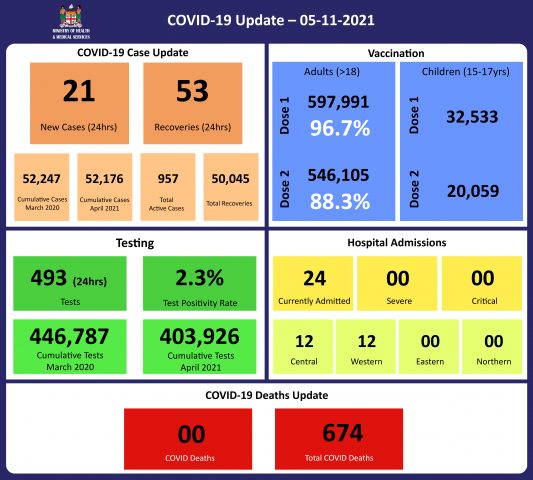
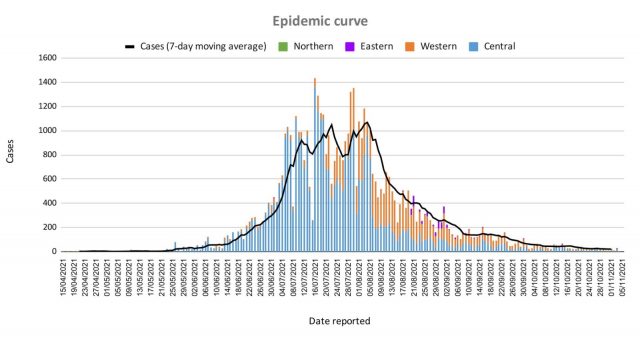
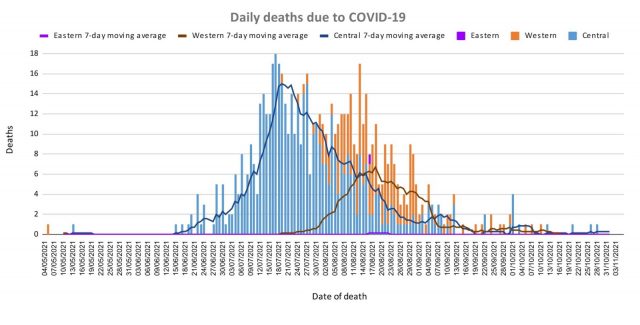
The Ministry of Health continues to monitor the outbreak using indicators such as daily case numbers, hospitalisations, test positivity, and deaths. There is a downward trend across all indicators of the COVID-19 epidemic in Fiji, indicating a positive response to our overall COVID containment and mitigation response.
Occupancy rates in health facilities, the occupancy rate of ICU beds, death rates, and vaccination coverage are indicators to monitor our health response capacity and we see a decreasing trend across indicators from our health facilities with increasing vaccination coverage for adults and 15-17-year-olds in Fiji.
Our weekly testing numbers of over 6,000 are still above the WHO recommended rate of 4 tests per 1,000 population per week (or approx. 3,500 tests per week) and we anticipate continued surveillance and testing in our communities and maritime islands to monitor and detect cases for early intervention.
Public Advisory:
A disease becomes endemic when it is expected to remain persistently present in the community. Some diseases endemic to Fiji are dengue fever and the common cold. These diseases persist at some level in the community and become epidemic when levels go beyond what is determined to be expected and acceptable. Determining what that acceptable level of disease is for COVID-19, is a work in progress but in general, it will be at the level which triggers additional control measures, Because COVID-19 is a vaccine-preventable disease, and the vaccines are very good at preventing severe disease and death, in a highly vaccinated population determining and monitoring acceptable levels, or thresholds, goes beyond case numbers. A disease that causes frequent cases in the community (like the common cold) but has a small impact on the numbers of people needing hospitalization or death, and minimal impact on the health system, will require less intervention. This is why we will be closely monitoring the following indicators: cases, test positivity, hospitalisations, and deaths.
Unfortunately, vaccine-related herd protection is not likely to be as efficient with COVID-19 as seen with some of the traditional vaccine-related diseases like measles. Recent data verified and released by the CDC indicate that unvaccinated people with the previous COVID-19 infection were 5 times more likely to have a positive COVID-19 test compared to vaccinated people. As such unvaccinated people cannot rely on herd immunity (or herd protection) nor natural immunity to protect themselves. Those eligible must get vaccinated to reduce their risk of infection, severe disease, and death. And we know vaccines are very good in preventing severe disease and deaths.
This lower efficiency in vaccine-related herd immunity also means that the public will need to live with COVID safe measures of masking, hand washing, physical distancing, and good ventilation and/or air cleaning technology. These COVID safe measures remain vital in preventing the need to go back to severely restrictive public health measures.
Supporting School Re-opening
COVID-19 poses a lower risk to children however secondary transmission from young school-age children can and does occur in both household and school settings. As school reopening continues, we will expect to find children with COVID-19 symptoms who will test positive. In these instances, an initial investigation will involve:
- Establishing whether or not the test reflects an old infection wherein the student is not infectious or a recently acquired infectious case.
- A review of the school covid safe conditions
- Initiation of the contact tracing investigations which will include immediate swabbing of high-risk contacts
Further actions will be dictated by the findings of this investigatory process. With good vaccination coverage and high levels of COVID safe adherence, it is possible for us to facilitate a measured containment program whilst continuing the school program. It is expected that these cases will help to refine the implementation of COVID safe measures in schools and help to put in place a quality improvement framework around the program to promote the safe opening of schools.
A recent case highlighted in the media is under investigation. Our initial findings suggest that this was a historical case and that the symptoms are unlikely to be related to COVID-19. We further confirm that no urgent measures were required immediately.
A more comprehensive report will be released once investigations are complete.
Students are reminded again of the need to maintain proper masking practices at all times, remain as much as possible in open ventilated spaces when with their friends, and follow all covid safe measures especially when indoors.
Travel to the North
For the North, the Ministry of Health and Medical Services is supporting a repatriation program and not a social travel program. As such travel for short-term goals is likely to be adversely affected if a person turns out positive while in quarantine. We are doing all we can to improve vaccination coverage in the North and we will review these quarantine measures for local travel after the 11th of November.
We are currently having a logistical challenge in providing the support for testing during quarantine because of the large volume of social travelers that have inundated the repatriation program. We ask those travelers undergoing quarantine in the North to be patient as we continue our protocols to protect the North while the vaccination program continues its rollout.