Last Updated on 2 years by Publishing Team
COVID-19 Situation Update
Friday 04th February
| Transmission Update:
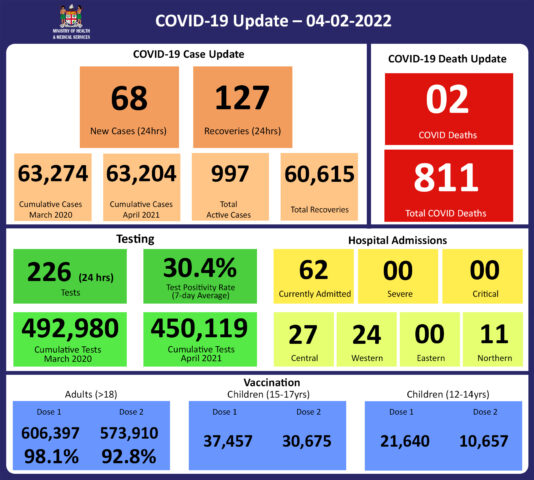
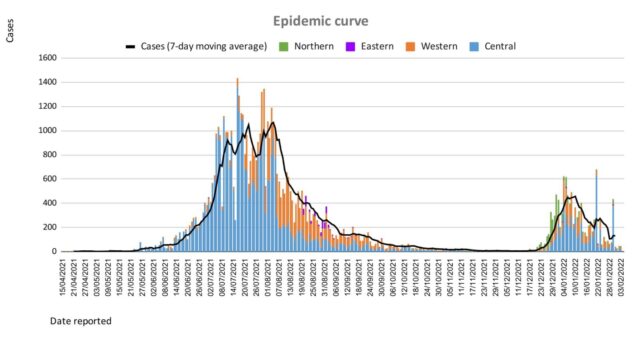
Since the last update, we have recorded 123 new cases of which 55 new cases were recorded on 03/02/2022 and 68 new cases in the last 24 hours ending at 8 am this morning. Of the 123 cases recorded, 50 cases were recorded in the Central Division; 53 cases were recorded in the Western Division, 20 cases were recorded in the Northern Division, and nil case was recorded in the Eastern Division. Overall, there have been 63,204 cases of COVID-19 recorded in Fiji, with 68% of the cases from the Central Division, 28% of the cases from the Western Division, 1% of the cases from the Eastern Division, and 3% from the Northern Division. The national 7-day rolling average of cases as of 31st January is 130 daily cases. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Deaths:
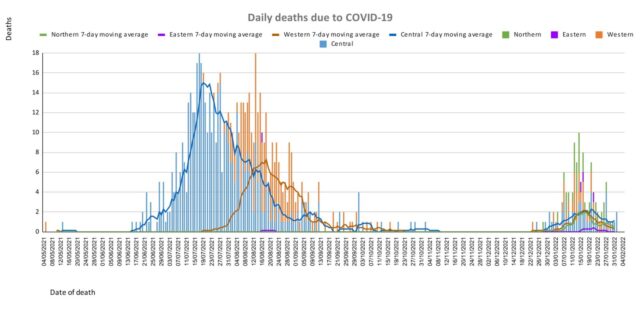
This curve depicts daily deaths by division since May 2021. (Please note: Death notifications from the week of 24/01/22 are still being received and we are currently on week 31/01/22 which is yet to be completed, therefore the appearance of a downward trend on the graph from week 24/01/22 may not be accurate. There are deaths from the Western Division currently under investigation for the same time period hence, the death rate for the division may increase). Analysis of Deaths in the Third Wave Table 1: Death rates by Division
An analysis of the 115 deaths recorded in the third wave show that, while the Central Division has the highest absolute number of deaths, the Northern Division has the highest rate of death when adjusted for population.(Note: There are deaths currently being investigated from the Western Division for the same time period, therefore the rate for the division may increase). Table 2: Deaths by Age Group
For the 115 deaths in the third wave, the rates of death when adjusted for population, have been highest in the age groups 50 and upwards. There were 7 deaths below the age of 19 years, 6 out of the 7 children had significant pre-existing medical conditions, and one child had no known underlying medical condition. Table 3: Deaths by Vaccination Status
Out of 115 COVID -19 deaths reported in the third wave, five (5) deaths were from the population not eligible for vaccination (under age 12). An analysis of the 110 deaths from the vaccine-eligible population reflected that when adjusted with per 100,000 population in fully vaccinated (received 2 doses) and unvaccinated/not fully vaccinated (received 0 doses or only 1 dose) adults in Fiji, a death rate of 8.1 per 100,000 population for fully vaccinated adults and 137.8 per 100,000 for unvaccinated adults was exhibited. This means that unvaccinated adults in Fiji have been dying from COVID-19 at a rate 17 times higher than fully vaccinated adults during this current wave. Individuals of the 12-17 age group who died were not vaccinated. There have been no COVID-19 deaths in individuals who received a booster (3rd dose) of the vaccine. New deaths to report There are 2 new COVID-19 deaths to report from 26th January and 1st February 2022. The first COVID-19 death to report is of a 2 month-old male infant from the Northern Division, who died at home on 26/01/2022. A thorough investigation was carried out by the Ministry of Health and the Police Forensics Unit, as a result, the infant’s death was classified as COVID-19 related. He did not belong to the population age group for vaccination hence, he was unvaccinated. The second COVID-19 death to report is of a 70-year old male from the Central Division, who died at home on 01/02/2022. He was fully vaccinated. There has been a total of 811 deaths due to COVID-19 in Fiji. Please note that due to the time required by clinical teams to investigate, classify and report deaths, a 4-day interval is given to calculate the 7 days rolling average of deaths, based on the date of death, to help ensure the data collected is complete before the average is reported. Therefore, as of January 31st, 2022, the national 7 days rolling average for COVID-19 deaths per day is 2.2, with a case fatality rate of 1.32%. We have recorded 849 COVID-19 positive patients who died from other serious medical conditions unrelated to COVID-19; their doctors determined that COVID-19 did not contribute to their deaths, therefore these are not classified as COVID-19 deaths. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Hospitalization:
There is a downward trend in daily hospitalisations. Using the WHO clinical severity classification, a greater percentage, 42% (n=260) of the admissions of COVID-19 positive patients are categorized as asymptomatic and mild,27% (n=17) are categorized as moderate and 26% (n=16) as severe with 3 cases in the critical category. Anyone admitted to the hospital is tested before admission, therefore, a significant number of people are admitted to the hospital for non-covid health conditions, but incidentally, test positive due to the high amount of transmission in the community. The number of people being admitted because of COVID-19 remains low. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Testing:
226 tests have been reported for February 3rd, 2022. Total cumulative tests since 2020 are 492,980 tests. The 7-day daily test average is 281 tests per day or 0.3 tests per 1,000 population. The national 7-day average daily test positivity is 30.4%. The high positivity rate is an indication of widespread community transmission. |
Public Advisory:
The death of the 2-month-old child at home continues to remind us that severe rare outcomes become visible every time we allow the transmission to run rife among us. As such we cannot afford complacency in our Vaccine Plus endeavour. We must do our best to protect the vulnerable by following COVID safe measures, getting fully vaccinated, and getting the booster dose when eligible (at least 5 months after the second dose). The evidence internationally, including from the United Kingdom, is that a booster dose (3rd dose) improves protection against symptomatic disease, which is reduced with infection with the Omicron Variant among the fully vaccinated and those previously infected with other variants. Studies are also showing that increased protection against symptomatic disease also decreases the risk of transmission to others, therefore, protecting the vulnerable.
As we see a reducing trend in transmission, we anticipate the trends in deaths also to follow suit. We will also, therefore, expect the reduction in COVID restrictions to help improve further our social and economic recovery. The public of Fiji is reminded, however, that we should expect the virus to be endemic, and for as long as the virus remains in our midst, there is always the risk of resurgence. As such, the vulnerable and relatively immobile minority population will still depend on the more immunocompetent and mobile majority for protection, both in maintaining the drive towards 100% vaccination of eligible adults and in adhering to their personal COVID safe behaviour measures. The tragedy of the deaths from COVID-19 is a sad reminder of the impact of this pandemic, however, the bigger tragedy is if all the very obvious lessons we have repeatedly published, announced, and posted on social media are too quickly forgotten. The Vaccine Plus approach must become a personal daily objective and the COVID safe measures become a community-wide habit, for us to safely navigate to a more secure socioeconomic future.
While we have reported that fully vaccinated people have died during this third wave, deaths in unvaccinated people (in the vaccine eligible population) are occuring at a massive 17 times the rate of the vaccinated. This confirms what we already know from other countries, which is that vaccination reduces the risk of severe disease, hospitalization, and death from COVID-19. The fact that we still have people not fully vaccinated, especially people who are at high risk of severe disease and death (the elderly and people with chronic diseases including NCDs) remains a serious concern. And we would strongly urge everyone, especially medical professionals, to encourage vaccination.
We have noted how difficult it is to increase our vaccination coverage for the last 10% of our adult population despite the increased risk of severe outcomes in this group. While we will continue to do our part to promote and deploy vaccines, we need community support to sustain the impact of our efforts especially to the vulnerable within this 10%. It is a grave concern that we continue to receive requests for vaccine exemption from persons with medical comorbidities, especially NCDs; their medical condition is an indication for vaccination, and granting the exemption is not an option for any qualified medical person.
The booster dose program began at the end of November 2021. As of January 31st, 78,806 individuals have so far received booster doses of the Moderna COVID-19 vaccine. For the month of February, a further 175,558 have become eligible for booster doses.
Health Services Transition
The implications of COVID-19 to health service provision are clear. The required change in the health service delivery model implies a change to infrastructure, human resource structure, working conditions, equipment, and the supply chain of drugs and consumables.
One important change that will require community-wide support is in developing the capability to ensure that available health care services get to those who need the service. Working with key partners such as WHO, UNDP, UNICEF, the World Bank, and other organizations such as Diabetes Fiji Inc, Fiji Cancer Society, Medical Services Pacific, Empower Pacific, Lifeline Fiji, National Committee On Preventing Suicide, and the Substance Abuse Advisory Council, we have evolved a network of avenues to help to provide prevention and care services for NCDs. We will continue to collaborate with other ministries and work with faith-based civil society organisations to enable our reach into communities.
With the pandemic into its second year, the Ministry has maintained emergency mode operations for much of this time. And as highlighted by WHO, there is data to show that more than 1 in 4 health workers globally has experienced mental health issues during the pandemic and several countries have reported that many health workers have considered leaving or have left their jobs because of difficult working conditions, staffing constraints, and the distress of making life and death decisions every day under intense pressure. There is an urgent need to safeguard the welfare of our medical staff by ensuring that they get some rest and attend to family needs. As such we will embark on initiatives to ensure that our staff move back to working normal working hours, take official leave entitlements accrued over the past year, and receive payment of meal and other allowances they are entitled to. We will continue to look at sustainable options to support our medical staff in working within the scope of our remodeling of health service delivery. However, we do anticipate that this will need to be part of a medium to long-term plan for the Ministry.
We have also highlighted how severe comorbidities and poor health-seeking behaviour have vastly contributed to severe outcomes in the COVID outbreak. We need to build resilience in the face of an endemic problem. Based on the lessons learned from the deaths, we need to:
- Prevent all preventable chronic diseases of which NCDs are the most prominent
- Promote the better control of controllable chronic diseases of which NCDs are the most prominent, and
- Build stronger support for better health-seeking behaviour especially among the vulnerable amongst us
We are urgently reviewing and strengthening our public health measures to find, stop and prevent health threats wherever they arise. Much of this will depend on a coordinated effort to detect these health threats early, investigate and put in control measures early. The Medical Sub-divisional Teams have been reminded to review and strengthen their community surveillance program and line list management of vulnerable persons.
However, the impact of these efforts cannot be sustained unless we get a broad level of support from the community in implementing the above 3 strategies, and at the same time reducing the transmission of COVID-19 to protect our vulnerable populations. Maintaining the Vaccine Plus approach remains critical.