Last Updated on 2 years by Publishing Team
COVID-19 Update
Thursday 04th August
| Transmission Update:
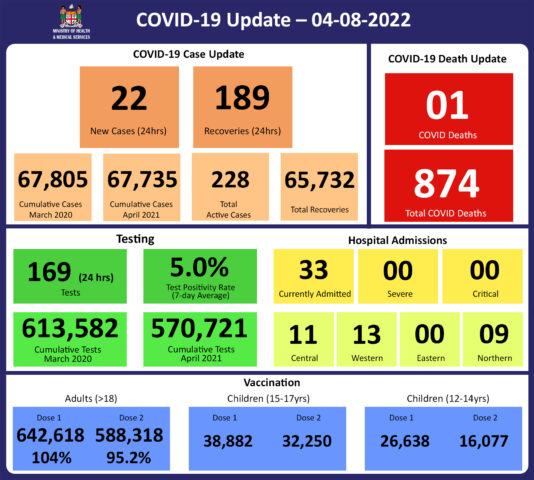
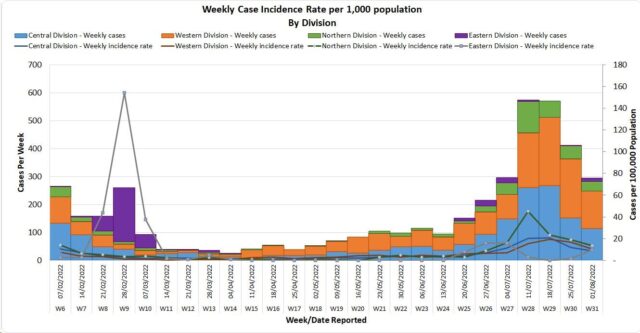
Since the last update, we have recorded 141 new cases of which 60 new cases were recorded on 02/08/2022; 59 new cases on 03/08/2022 and 22 new cases in the last 24 hours ending at 8 am this morning. Of the 141 cases recorded, 57 cases were recorded in the Central Division; 71 cases were recorded in the Western Division; 13 cases were recorded in the Northern Division and nil cases were recorded in the Eastern Division. The national 7-day rolling average of cases as of 31st July is 43 daily cases. In the 7 days until 03/08/2022, 92 new cases were recorded in the Central division, 100 new cases in the Western division, 18 new cases in the Northern Division and nil new cases in the Eastern Division. The Central Division cases constitute 66% of the cumulative total cases nationally, with the Western division making up 28%, 4% in the Northern Division, and 2% in the Eastern Division. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Deaths:
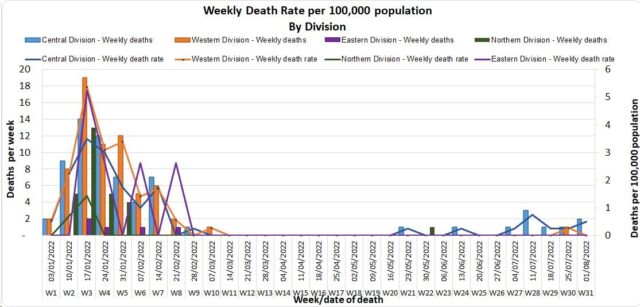
The curve depicts weekly COVID-19 deaths by division since May 2021. It indicates a surge from last December, with peaks in mid-January 2022 followed by a downward trend. The latest COVID death was reported on 27/07/2022. COVID Death Reports We have one COVID-19 death to report. An 88-year-old female from the Central division died at home on 14/07/2022. She had multiple pre-existing medical conditions and had received two (2) doses of the COVID-19 vaccine. Analysis of COVID-91 Deaths Table 1: Death rates by Division
An analysis of the 173 deaths recorded since December 2021, shows that the Central Division has the highest absolute number of deaths, and the Northern Division has the highest rate of death when adjusted for population. Table 2: Deaths by Age Group
For the 173 deaths since December 2021, the death rate adjusted per 100,000 population, has been highest in the age group 50 years and over. There were 8 deaths below the age of 19 years, 7 out of the 8 children had significant pre-existing medical conditions, and one child had no known underlying medical condition. Table 3: Deaths by Vaccination Status
Out of 173 COVID-19 deaths reported since December 2021, six (6) deaths were in the population not eligible for vaccination (under age 12). An analysis of the 167 deaths in the vaccine-eligible population revealed that Fiji has a death rate of 11.3 per 100,000 population for fully vaccinated adults and 328.2 per 100,000 population for unvaccinated adults. This means that unvaccinated adults in Fiji have been dying at a rate 29.0 times higher than fully vaccinated adults. Individuals in the 12-17 age group who died were not vaccinated. There is one (2) individual who recently died due to COVID-19 and had received the 3rd Booster dose. There has been a total of 874 deaths due to COVID-19 in Fiji. As of July 31st, 2022, the national 7 days rolling average for COVID-19 deaths per day is now 0.3, with a case fatality rate of 1.29%. Due to the time required by clinical teams to investigate, classify and report deaths, a 4-day interval is given to calculate the 7 days rolling average of deaths, based on the date of death, to help ensure the data collected is complete before the average is reported. We have also recorded 969 COVID-19-positive patients who died from other serious medical conditions unrelated to COVID-19; their doctors have determined that COVID-19 did not contribute to their deaths, and therefore these are not classified as COVID-19 deaths. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Hospitalisation:
Using the WHO clinical severity classification, there are 73% (n=24) cases in the asymptomatic and mild categories; 24% (n=8) in the moderate category; nil cases in the severe category and 3% (n=1) cases in the critical category. Anyone admitted to the hospital is tested before admission, therefore, a significant number of people who are admitted to the hospital for non-covid health conditions, test positive for COVID-19 due to the current level of transmission in the community. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Testing:
169 tests have been reported for August 3rd, 2022. Total cumulative tests since 2020 are 613,582 tests. The 7-day daily test average is 1,234 tests per day or 1.4 tests per 1,000 population. The national 7-day average daily test positivity is 5.0% which is borderline with the WHO recommendation of 5%. |
Public Advisory
For COVID-19;
As reported earlier, we continue to see a concerning trend in COVID-19 cases. Whilst there is some decrease in the reported data which is supported by other community-based indicators we continue to be vigilant. The death reported today demonstrates the recurring theme that our vulnerable persons need close oversight and early hospital intervention. We need to escalate community-wide adoption of COVID safe measures together with immunisation.
Hospitalisation for severe diseases remains within manageable limits. While BA.5 has the ability to evade immune protection against infection induced by prior infection and/or vaccination, – there remains significant protection against severe disease, and there is no evidence that BA.4 and BA.5 cause more severe disease than previous variants. Vaccination combined with COVID safe measures will ensure that the health care load remains manageable.
Our hospitals have reintroduced stringent COVID safe measures which include restricting visitors, and more strict enforcement of masking, and hand sanitization practices while strengthening screening protocols. For workplaces, we strongly advise that COVID safe measures be more actively promoted and enforced by management.
Community and Workplace leaders must bring back many of the COVID safe measures that your community and/or organisation has learnt during the acute outbreak. We need to be able to live with COVID by reducing the risk of vulnerable people getting COVID and/or suffering from severe consequences. COVID safe measures prevent us from getting COVID and reduce the risk of spreading to the more vulnerable in the community.
We have maintained a number of public health mandates and measures related to vaccination and incoming travel. The Ministry of Health and Medical Services envision that the more people get vaccinated with the booster doses, the better the level of protection, and the safer it will be to remove the remaining public health measures further. For this to happen, the Ministry is currently targeting an 80% booster coverage for those over 18 years of age. We may review this threshold if current trends in cases and severe disease hold.
Anyone who is sick should not be attending work or school. If you have COVID-19 symptoms, you must get tested for COVID-19. If you test positive, isolation is mandatory for 7 days.
COVID-19 Vaccination
We have been reporting that 100% of our estimated adult population have received one dose and at least 95% have received the second dose. The vaccination of our target population has been progressing well with the 12 years and above coverage rate for Fiji being 99% for Dose 1 and 89% for Dose 2. Furthermore, as of the 01st of August, a total of 156,581 (50%) booster-eligible individuals have so far received their 3rd dose while 19,673 individuals have been administered the 4th dose.
Increasing Vaccine Booster Coverage Program
We urge the public to get booster vaccine doses with a list of vaccination sites provided daily by the MHMS. Currently, both Pfizer and Moderna are recommended for booster doses.
In order to optimise coverage, the aim of the booster campaign is to administer 250,000 doses of Pfizer vaccine to those who have completed the primary series (doses 1 and 2) > 3 months prior but have not yet received a booster dose.
COVID-19 booster priority populations are;
- Persons over the age of 18 years who have completed their primary series > 3 months prior can receive their 1st booster dose
- Immunocompromised persons and those over the age of 60 years who had received the 3rd booster dose, may receive the 4th dose after a period of 4 months
- Health care workers, port staff, tourism and others who wish to receive a 2nd booster dose may receive it after an interval of 4 months from their first booster dose.
- Anyone over 18 years who have taken their 1st booster dose can receive a 2nd booster dose after an interval of 4 months.
COVID-19 vaccination to the 5-11 years in Fiji.
Overall Plan
The Vaccination Roll was started in the Central Division on Wednesday 6th July. While we had hoped for rapid and broader deployment the stringent cold chain logistics need further strengthening to support further deployment, to the Western Division then Northern and Eastern Division.
The Ministry of Health and Medical Services is committed to:
- Equitably allocating sufficient doses to vaccinate all the 132,893 children aged 5-11 in Fiji.
- Equitably track and position vaccine sites to ensure that eligible individuals can receive vaccines in a safe and timely fashion.
- Provide evidence-based, unbiased information on vaccine safety, physical distancing, and mask-wearing to maximize the impact of these vaccines.
The Fiji Action Plan for COVID-19 vaccination of children aged 5-11 is a three-fold approach to;
(1) Identify and prioritize eligible individuals and communities,
(2) Engage those individuals and communities with a targeted outreach and communication plan and,
(3) administer the vaccines.
Administration of Vaccine
The Ministry of Health and Medical Services through the 22 Sub Divisions with our School Health Teams have been leveraged to carry out the planned Vaccination rollout.
All school sites have been contacted to be vaccination sites.
The Health Facilities will also host vaccine clinics, as well as Pfizer vaccine clinics on weekends and the School Holidays.
The Sub Divisional Mobile Teams will also implement a homebound vaccination program that will be available to ensure that homebound children aged 5-11 will have access to immunizations if not available through their Schools.
Vaccine Clinics
Sites that have been identified for the administration of the Pfizer-BioNTech vaccine include:
- Current Fixed MCH clinics operated daily for those children of 5-11 years who would want to access these facilities.
- Mobile vaccine clinics for the Early Childhood Education Centres.
The School Vaccination Teams will be visiting schools this Term 2 to conduct vaccination according to the planned dates.
Other schools identified as priority community vaccination locations include the special schools that cater for children with special needs.
Opportunities may be offered to the sites hosting community events (sporting, etc.)
The Consent Process
Consent is obtained through the Consent Form of a parent or guardian for allowing their child to receive the age-approved vaccination.
The consent process includes;
Onsite consent to be provided by a parent or guardian who is physically present with the minor at the vaccine site. The parent or guardian will sign an appropriate vaccine administration Consent Form.
For Off-Site consent:
- A consent form can also be taken home by children to be signed by the parent or guardian
- A letter can also be written/typed and signed by the parent or guardian.
- The acceptance of a letter of consent must be documented by the Vaccination Team and the letter should be retained with the patient record.
- The presence of a support person will be accommodated at all vaccine sites
Consent and Vaccine Information Documentation:
The Consent Form includes information on demographics (name and DOB), questions asked by the parents or support person and a place for the parent/guardian’s signature. Your questions will be dealt with by the vaccine provider.
The Vaccination Card indicates approval to release identifiable information to medical providers, and a place for the vaccinator to note the date (1st and 2nd Dose), a batch number and the type of vaccine.
A vaccine information booklet accompanies the Consent forms.
Non-Covid Vaccine-Related Immunisation
Globally, WHO has expressed concern regarding falls in non-covid immunisation rates due to the pandemic. We have seen this manifest in a number of developed countries. We also expect that certain areas in Fiji have immunity gaps. In addition, we have reported suspected cases of measles (8) and rubella (2) wherein the initial tests done were positive. We have also been made aware that a number of circulating viruses can result in false positive tests for measles and rubella. Despite this, we are currently conducting preventative Supplementary Immunisation Activities throughout the nation to mitigate the potential impact of these reported cases.
Monkeypox
The WHO’s Director General has declared the monkeypox global outbreak a public health emergency of international concern. At the time of the announcement on Saturday, July 25th there were over 16,000 cases reported to WHO from 75 countries, with the most reported by countries in Europe, followed by the Americas. The 5 deaths reported had occurred in African countries previously endemic to monkeypox. The announcement of a public health emergency of international concern was made recognizing the complexities and uncertainties associated with this public health event, and to alert countries to urgently take recommended actions based on their epidemiological situation, patterns of transmission, and capacities. As we have not detected a case, Fiji is classed in Group 1: States Parties, with no history of monkeypox in the human population or not having detected a case of monkeypox for over 21 days.
Monkeypox is usually a mild and self-limiting illness, which means that most people recover with just supportive (symptom relief) treatment within several weeks. However, previous outbreaks in endemic African countries have demonstrated that severe illness can occur in some individuals, including those with compromised immune systems, young children, and pregnant women. We are in discussions with development partners to see if we can preposition access to vaccines and medications used to treat monkeypox.
We are also aware that the monkeypox transmissibility is much lower compared to COVID-19, with the current evidence being that transmission occurs through direct physical contact, respiratory droplets, or contact with items that may have had contact with the lesions of an infected person, such as their clothing or bedding. As such, it is more amenable to the border and community-wide containment measures we currently have in place.
As previously mentioned, our response plan includes surveillance with rapid response and containment protocols. A key focus will be on ensuring that those suspected or confirmed to have monkeypox must be managed in a dignified manner and without any stigmatization. Each citizen’s duty to contribute to protecting Fiji must be the priority. The WHO statement clearly highlights the negative role that stigmatization plays in early diagnosis and containment.
As part of our ongoing response, the Ministry of Health and Medical Services continues screening and symptom monitoring of people arriving from a list of countries with evidence of community transmission of monkeypox. People arriving in Fiji from these countries have been monitored for symptoms and followed up by our health teams until 21 days after their arrival.
We are developing activity plans to engage key community-based groups, and civil society networks to increase the provision of reliable and factual information about monkeypox to populations that may be at increased risk of infection.
The Ministry has published a number of public advisories to help arm ourselves with the knowledge to protect ourselves and to help reduce the chances of spread in our community. Infection prevention protocols have been put together at the border and in community health facilities. The public advisories have covered symptoms to enable the public to quickly seek medical care while preventing transmission to others.
All doctors and nurses in the community need to ensure they are well informed of how cases present and be vigilant in helping cases get diagnosed early. The Ministry’s guidelines for early detection and response, as well as laboratory testing, have been distributed to public and private clinicians. And clinician awareness sessions have also been conducted.
We are currently awaiting testing supplies and expect to soon begin testing for monkeypox at Fiji CDC. Our ongoing efforts to develop genomic sequencing capability at Fiji CDC will also provide us with greater capacity to deal with infection threats now and in the future.
As we escalate our community-wide infection prevention and control measures, we are responding to current threats and creating community-wide resilience to upcoming threats.